Prostate Cancer
A Lifetime of Good Health Ends
|
You should know as you're reading this account of my prostate cancer that I am not a medical professional.
The information about the disease I give here has been researched, but I can't pretend all of it is accurate.
Also, throughout this account I will be sometimes very critical of some of the doctors that treated me. But that doesn't mean I don't necessary think they are bad because if I've learned nothing else I have come to the appreciation of their care noting that they must navigate both liability and insurance. Know that I am not revealing the true names of any of the health care professionals and when I do specify a name unless I specifically state it, know that it is an alias. Finally, I believe I now have additional appreciation of the complexity of the human body. It's not only incredibly complex, it seems like it was designed from the pen of Rube Goldberg. You should value whatever health you have because the body is so complex it's nothing short of a miracle that it ever works! |
Background
I've enjoyed a lifetime of really good health. So much so I remember those times when I wasn't without difficulty. I wasn't sick very much and my attendance from 7th grade through the end of high school was just 4 and half days missed. I say the number confidently because in 7th grade I didn't miss a single day of school so started to track it. In 6th grade I missed several days because I got the flu.
I did have one cracked rib from playing football in 8th grade, but I played for an entire week before it was diagnosed. And one physical I took in 9th grade was by a doctor who specialized in heart issues discovered I have a heart murmur. My mom was obviously concerned about that but the doctor assured my mom it was trivial and shouldn't ever prevent me from any physical activity. Throughout my life most doctors have failed to hear it so it is always striking to me when they do. I can tell because they're taken aback and I can see them struggling, seemingly trying to find the right words. I always smile at them and say, "You heard the murmur!" and it looks like a weight has been taken off their shoulders because this is not news to me. As I've gotten a lot older it must be getting stronger because it gets detected more often.
My first real medical issue came in 1985 when I got a hernia which was bad enough it needed addressing. It wasn't always out, but when it was it was obvious and I remember one time playing tennis I had a strange feeling and so I knew I better take care of it immediately. A visit to my General Physician, Dr. Gilbert (real name), was a little disconcerting. It wasn't out at the time and gave me the standard "turn your head and cough" which I had done enumerable times in my life. He felt nothing! But he said I must have one because of my description. Sure, all those "turn and cough" tests were practically worthless. He referred me to a thoracic surgeon (Dr. Roger Wilcox - real name) who was just one floor below. This was a very memorable visit as he had various photos on the wall showing he'd served in the military. A tennis friend who was nurse said of Dr. Wilcox that he is a genuine "Hawkeye Pierce." I looked him up recently and this is from his obituary as he died in 2006:
"Re-enlisting in the Army in 1951, he served for 19 months in Korea at the 8063 M.A.S.H. and achieved renown both as a surgeon and as a personality, with some of his exploits immortalized in the book, movie and TV series M*A*S*H."
Of course I have to drop my pants and I think I'm going to get the standard turn your head and cough, but Wilcox reached into my groin with 4 fingers and lifted so hard it felt like I could have come off the ground. He immediately says, "Yes, you've got a hernia." The discussion about the surgery was pretty short, but the memorable part was Wilcox said he could do the surgery using just a local or going fully under (general anesthesia) with an anesthesiologist. My response was immediate as I had already given it thought and said, "Why wouldn't I choose the local? Isn't all the risk of this surgery in the anesthesia?" He simply said yes and he seemed happy with my choice.
The surgery went well and though I only had a "local" I never really heard a thing. They had this blanket/sheet above me so I could only see a small part of the ceiling. Every so often I remember a nurse sticking her head in and asking, "Are you okay?" I have no idea if I even answered. But when you exit the operating room you're fully conscious and they wheel you down to the recovery room. I was offered apple juice and they were just observing me to be sure I was okay to be released. While I was there, however, I got to see two different people who had general anesthesia (GA) awake and they flailed around from disorientation. I didn't know why at the time, but this would weigh on my mind later as I learned that under GA you don't dream so you don't experience the passage of time. I met with Dr. Wilcox 5 days later and pronounced that I was good and could do any physical activity, including no lifting restrictions.
Another Hernia
Some 20 years later in 2006 I got another hernia, this time on my right side. I knew this was probably inevitable because if you have a weakness it will generally be on both sides. As I was still very physically active, ignoring it was not an option so it was off to the doctor for a referral. Meeting with this surgeon (whose name I can't remember for sure but I think it was Kevin McGeever) laparoscopic surgery was now available and this doctor recommended it over the classic surgery. He said I'd recover much quicker than my first, but seemed genuinely surprised when I told him I was given the a-okay after 5 days. There was, however, a downside in that the laparoscopic surgery required general anesthesia because they have to blow up the stomach to make room. I cringed a bit but decided I'd go with his recommendation. I'm really healthy so what really could go wrong?
The prep for this hernia repair was very much the same, but with the difference of meeting the anesthesiologist who would introduce himself and finally giving me the injection which would put me to sleep. I thought it appropriate that I give him a heads up that I might not be his usual patient. I told him I don't smoke (never have), don't drink (never have), never taken narcotics, and simply don't take any medications, not even aspirin. I was worried that I might have a strong reaction to the anesthesia, but he reassured me that it wouldn't be an issue. Interestingly, before he gave me the injection, he gave no warning about what was about to happen, but I had already researched it and knew that just moments after the shot, I would almost instantly be in the recovery room. For with GA you don't dream so don't experience the passage of time *.
And instantly I was in the recovery room, not entirely conscious, but feeling the inflation of a blood pressure cuff on my left arm. It made perfect sense as they would be taking my blood pressure. After the cuff deflated I managed to ask the attending nurse, "What was the reading?" I can't remember the exact numbers, but it was something awful like 50 something over 30 something. My response was, "That's too low!" and I fell back to sleep. When I awoke again it was for good, but I kept asking for the reading and the next one was something like 60 over 40. Not great, but better and going in the right direction. Then I see my anesthesiologist walking by. He looks over in my direction, but doesn't stop. Then I see him walking back the other direction and once again just glances over. He would do this again so now I knew my situation wasn't normal. He was worried. I don't know why he didn't stop, but I think all he was doing was getting signals from the nurse that I was progressing in the right direction. I would see him do this walkby 2 more times.
It took 2 and a half hours to get released when normally the time is just under an hour. My ex-wife, Cindy, was with me and when she met me with the attending nurse she was given a pain medicine prescription with the warning about the pills, "Watch out with him. I little goes a long way!" But the pills weren't an issue because I didn't need any pain relief!
* The passage of time is part of good brain function. At my very first Alzheimer's evaluation one of their questions was, "What time is it right now?" You had to answer without relying on a watch or your phone. I only briefly thought about it and said, "9:15" and I was within 10 minutes of being right. Ever since then I've been obsessed with this concept. Almost every time I wake up in the middle of the night (usually because I need to go to the bathroom), I make a guess as to what time it is and I'm always amazed that I can guess it within 15 minutes, plus or minus. Only rarely am I off by an hour or more.
Debilitating Pain
 In December of 2021 there was an incident that happened while playing tennis at a nearby community. I'd heard that they had a great tennis
program, but no one said their courts were way too small. The marked court itself is always regulation sized, but the amount of space around
it can vary. And this community did not have enough room. So they had this barrier between the courts to keep balls from going on to the adjoining
court. Our courts have plenty of space and they have a fence to keep balls in the court. They had this triangular concrete wall between the courts
which was heavily padded in case someone were to run into it. Well I did: twice! Each time totally an accident. I was running for a ball that I
would otherwise easily get when suddenly the wall stopped me. This might have been absolutely nothing as I was fine, but near the end of the match I
could feel something in the upper right groin area and my thought was, "That's not good." But it didn't affect my play and during the weeks that
followed, but by January it became a big problem. I could understand a connection if I had hit that wall on my right side, but in each case it was my left.
In December of 2021 there was an incident that happened while playing tennis at a nearby community. I'd heard that they had a great tennis
program, but no one said their courts were way too small. The marked court itself is always regulation sized, but the amount of space around
it can vary. And this community did not have enough room. So they had this barrier between the courts to keep balls from going on to the adjoining
court. Our courts have plenty of space and they have a fence to keep balls in the court. They had this triangular concrete wall between the courts
which was heavily padded in case someone were to run into it. Well I did: twice! Each time totally an accident. I was running for a ball that I
would otherwise easily get when suddenly the wall stopped me. This might have been absolutely nothing as I was fine, but near the end of the match I
could feel something in the upper right groin area and my thought was, "That's not good." But it didn't affect my play and during the weeks that
followed, but by January it became a big problem. I could understand a connection if I had hit that wall on my right side, but in each case it was my left.
It seemed like a pulled muscle in my upper right leg fairly near the groin. It got so bad that getting into a car could be painful if I splayed my leg at all. Eventually I figured I had to stop playing tennis to get it better. And it did get better, but at a snail's pace. But I was able to play golf because I didn't have to twist my leg as that would be very painful. However, when our golf friends came out I now had a new problem: my shoulders were stiff and they were giving me pain. My right shoulder in particular was really bad and then my right wrist was having issues. I had some trouble on my left side, but it was minor compared to the left. That muscle near my groin which was always bad, weirdly, I would sometimes feel some pain on the left side! I guess it's a universal that if you are experiencing really bad pain in one area of your body, it can completely mask minor pain elsewhere. So as the leg got better this other stuff seemingly showed up. The other thing was I was feeling run down so I was tired. And I don't weigh myself very often, but when I finally did I had lost 12 pounds. Putting on socks in particular was horrible and it could ruin a day because it would trigger more leg pain. I was constantly reminded that you don't really appreciate good health until you don't have it.
We were supposed to be headed to Hawaii in late April for 8 nights. Suddenly Debbie announced we had to cancel the trip because of my health. I wasn't sure she was right, but I deferred to her judgment. I thought I was doing better, especially in my right leg. So with that decision we would do the big drive back to WI on the day we should have been leaving for Hawaii. So no possible Boom Boom Deck scenario. But with that decision I went back to trying tennis, even though I couldn't play nearly at the level I was used to. Debbie was a little dismayed that I appeared to be doing better, but I really wasn't. The difference was I was no longer worried about screwing up the Hawaii trip. I was now free to be more active! But things were far from good. Between the inability to raise my right leg and pain in my shoulders, putting on socks was a major daily project. She set up an appointment with a new doctor while still in AZ and good thing because they were booking 2 months in advance. Not great that it would be a new doctor because our old one moved to another state.
For the first time in my life I saw a chiropractor and she said that wall crash could be significant if there was a hip injury or caused a hip alignment problem. She did some work on it, but couldn't determine there was any problem. A couple of visits were all I had because we had to get back to WI, but I felt no improvement from the chiropractor visits.
"That's a rotator cuff injury."
Upon our return to WI, I finally got a visit to my new physician, Dr. Carl Smith, which will turn out to be a low point in the journey to get a hold of what was going on. Though he was very personable, he didn't listen to what I was saying at all. He had a very simple explanation for the pains: old age! Old peope get pains so get used to it. He did check my right shoulder and after moving it in only a couple of directions which was painful he said, "That's a rotator cuff injury, no doubt about it." Rotator cuff? That's terrible! First, you only have two options: (1) live with the pain as long as you can, and (2) surgery. But the worst part: what does that have to do with everything else that's going on? He said he would refer me to a Physical Therapist. After he did listen that I might have had a hip injury from tennis, he said that could explain a lot. He then sent me immediately to radiology to get a hip x-ray and a right shoulder x-ray and came back to see him when that was done. These days the x-rays are digital and my GP could call them up and check them himself, even though the official reading will come later with a radiologist. Smith looked at the x-ray and announced, "Yes, there it is," as he pointed to the area on the image. The official reading was "Moderate acromioclavicular DJD [Degenerative Joint Disease]" which I disagree (I think it's merely mild) because before and after this inflammation I've had no pain, period. So at best it would be mild. But looking at the hip x-ray he actually sounded disappointed as it looked absolutely normal. But had there been something there it would have explained a lot.
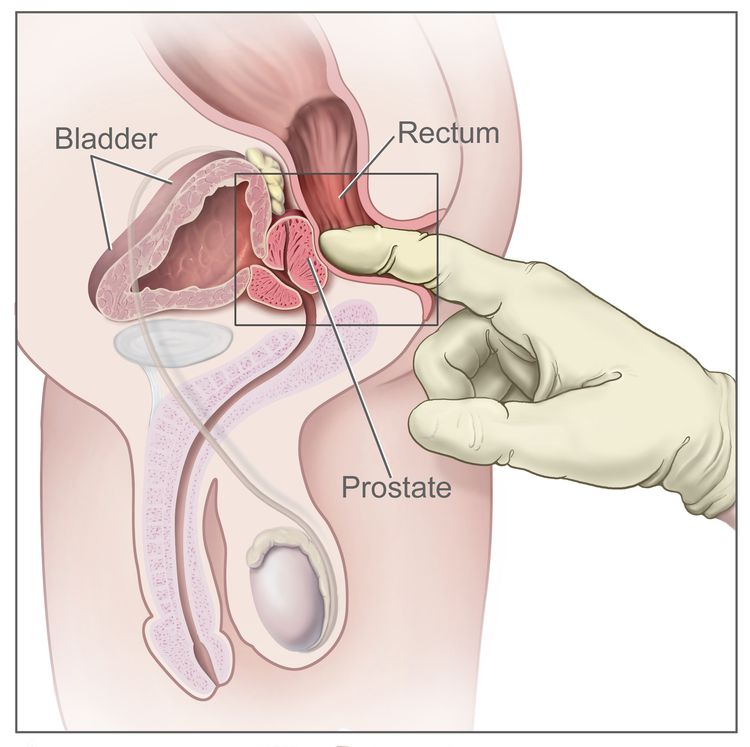 He then did a prostate exam (technically a Digital Rectal Exam) which was very painful and then announced it was
enlarged. That's another inevitability of age, and I've been tracking
that for the last 30 years. Yeah, I don't normally make it through the
night without needing to go, but when I need to go, I do need to go. So
now there's the ominous specter of prostate cancer. But he was really not
concerned and he didn't think anything needed to be done right now. It
was puzzling, but later with research I learned why. Enlarged prostates
in older men are the norm and doesn't mean you have or will get prostate cancer.
And that cancer itself is very slow to
grow. But Debbie was going to have none of that!
She was now like a dog on a bone and afterwards would insist on a follow
up appointment because of the specter of cancer.
He then did a prostate exam (technically a Digital Rectal Exam) which was very painful and then announced it was
enlarged. That's another inevitability of age, and I've been tracking
that for the last 30 years. Yeah, I don't normally make it through the
night without needing to go, but when I need to go, I do need to go. So
now there's the ominous specter of prostate cancer. But he was really not
concerned and he didn't think anything needed to be done right now. It
was puzzling, but later with research I learned why. Enlarged prostates
in older men are the norm and doesn't mean you have or will get prostate cancer.
And that cancer itself is very slow to
grow. But Debbie was going to have none of that!
She was now like a dog on a bone and afterwards would insist on a follow
up appointment because of the specter of cancer.
After this initial visit we came home and I was really depressed. I was no closer to an explanation of what was going on and now I have two new big potential problems. The rotator cuff was especially bad because the only thing you can do is live with the pain for a while, but eventually I would need surgery. The doctor did give me a referral to a Physical Therapist which I thought was needless because I thought what could the PT give me? In the two weeks that followed my condition got worse.
We needed a follow up appointment, but the earliest date was 6 weeks out. But we were offered an appointment with the doctor's Physician's Assistant (PA), Lucy Whitman. I had two previous experiences with a PA and they were both very positive. If I only had to judge things by those examples, I conclude they often give better care because they are much better at listening to a patient and they are far less arrogant.
So we were able to see the PA just a week later and it was a much better visit. The PA gave me another prostate exam (which was just as painful), and ordered the prostate blood test (PSA - Prostate-Specific Antigen). She said if that was bad I would get a referral to a urologist. I was now doing worse, so much so that now I could hardly play the piano which we pointed out to her. She had me grab both of her hands and told me to squeeze them as hard as I could. I assured her when I was healthy that she'd most likely be in pain if I did that. We were able to tell her the entire story and listened! She also ordered various other tests including some for inflammation. In her notes I read later her suspicion was that it was PMR - Polymyalgia Rheumatica, but the right shoulder was still problematic because it was so much worse than the left and with PMR the pain should be bilateral.
I then had another appointment with the PA about 2 weeks later. The prostate test was not good. The normal range is 0-4.5 and my reading was 12.85. I thought that sounded pretty bad. Consequently, I got a referral to a urologist. Most of the blood tests were fine, but two of them (ESA and CRP) which are tests for inflammation were extremely high. She still thinks it's PMR, but they apparently cannot directly diagnose that problem. They have to back into it by eliminating all other possibilities. Her thought was that it could be rheumatoid arthritis and even though she didn't think it would be Lyme disease, I got tested for both. Looking online both of those would explain a lot, although it wouldn't explain everything. Both tests were negative. But there was still the problem that the right shoulder wasn't quite fitting the inflammation picture as PMR is normally bilateral.
"I don't think this is a rotator cuff problem!"
On that same day I had my appointment with a physical therapist, Julie Munson, and it was not what I expected. I thought we'd be in the gym area and I'd be given a bunch of exercises. But instead it was almost entirely an office visit with the PT taking a large number of measurements on both shoulders so the movement restriction would be compared. 30 minutes into this examination she says, "I don't think this is a rotator cuff problem! There's too much that doesn't fit." Then she says, "I think it's Adhesive Capsulitis," and that meant nothing to me. But she added, it's normally called Frozen Shoulder. And get this: one of the usual sources of this problem is inflammation. Right there and then I'm doing a happy dance in my mind because 1) it's not a rotator cuff problem at all (i.e, no surgery) and 2) this now fits with most of the other stuff. Frozen shoulder she went on to describe as a good news / bad news situation. It gets better by itself, but takes anywhere from one to four years. I was still in the first phase where there is pain and no movement. The second phase the pain goes away, but still with limited movement. The third stage the movement gets better until you're fully recovered.
The other piece of great news out of the PT appointment was about exercising. No, I wouldn't be making things worse. the PT simply said do as much as you want or can. If it hurts too much, then stop. I don't know if it was all mental, but after that I just started feeling better in general and day by day my condition improved. I only know after the fact the reason was I could finally exercise with the confidence that doing so wasn't making my situation worse. I could have used this months earlier!
A few days later, the PA prescribed a 5-day supply of Prednisone which is a powerful anti-inflammatory steroid pill to see how I would react to it. I was warned about side effects and my research told me these are not to be taken any longer than humanly possible because the long term side effects are really bad. But the pills were nothing short of magic. Within a day almost all the issues vanished leaving me with only some residual stiffness in the right shoulder. I never knew that the simple act of putting on socks could be so satisfying. I also didn't realize that it was effecting my legs. I really dreaded the day I came off them because I feared all the pain and stiffness would return, and it did, in only a few days.
With that reaction I got the referral to the rheumatologist which was given to me the next day on a phone call from a nurse's assistant, and says the PA thinks I have Polymyalgia Rheumatica (PMR). I never heard of that! So off to the internet and what I read was pretty amazing. It checked almost all the boxes of my symptoms. It's not a joint problem at all. It's entirely muscles. PMR means "Many Muscle Pain." Suddenly my leg problem is related! Weight loss, fatigue, loss of appetite, pain in the neck, shoulders, and upper arms. They don't know the cause, but they think it's a yet to be identified virus. There is no cure, but it does get better in a 1 to 4 year time frame. I would only find out later I was wrong about that. It only starts to get better after a year.
Three weeks later I had a follow-up visit to the PT and after I said I seem to be doing a lot better, she started to make measurements of my motion without regard to what she'd measured on the first visit. She described this as a "blind test" and was surprised I knew what that meant. Comparing things she noted that almost everything showed a 40-50% improvement. She gave me some exercises and offered another follow up, but I didn't feel I needed it and in the end I was right. I was taking ibuprofen which was suddenly doing me a lot of good. When I was in AZ I had tried taking them, but I was convinced they were just placebos as they appeared to do nothing for me.
For my enlarged prostate and elevated PSA, my referral was to urologist, Laurie Schlesinger. This would be a good visit as I found her to be excellent and especially good at explaining things. Of course I had researched things and found that the only way they really know it's prostate cancer is through a biopsy which is expensive or an MRI which is even more expensive. But apparently the insurance companies frown on these for the most part doing other cheaper tests. That didn't seem to make sense. Don't you want to identify this as early as possible? Apparently not. The explanation I got was that the number of positive results from biopsies was small. And prostate cancer is not like most other cancers where it can spread fast. When my physician said I could wait until next year he wasn't wrong. But what about that high reading where mine was 12.85* and the normal range is 0-4.5? The urologist said that reading was still pretty low. She had patients with numbers higher than 900! However, she was more than willing to give me the biopsy, but it was entirely my decision. My thought was why not? She gave me a prescription for Flomax which is supposed to make urination easier, but to me it seemed like it was just a placebo. In a subsequent visit with Schlesinger she told me I could stop taking it if I felt it wasn't doing any good.
* My further research gives me more insight into the real issue which is PSA itself. It's actually in the name PSA - Prostate-Specific Antigen. It's made only in the prostate and a healthy one produces it. The upper limit of 4.5 is somewhat arbitrary. The presence of cancer usually but doesn't always elevate the level, and an enlarged prostate always raises the level. And I learned that an enlarged prostate is only occasionally related to cancer. The prostate normally enlarges as we get older. So PSA is a terrible indicator. Using it to screen for cancer causes many false positives and many false negatives. But it's used because there is no better relatively cheap substitute.
Alzheimer's

|
| Pam with longtime friend, Dawn, in March of 2022. |

|
| Me with Pam in April 2021. |
The pictures of Pam seen here show how devastating the toll the disease took on her appearance. She passed away on January 6, 2025 at age 70.
My status is uncertain. But I'm obviously more than a little paranoid. I can feel my cognitive skills starting to wane, but is that just the normal "getting old" decline? At the advice of a friend I signed up for the Alzheimer's study at UW and was accepted for the initial testing, probably because of the family history. I ran through the tests and then if they think I'm still a good candidate, about 2 months later they do an MRI of the brain and a perform a Lumbar Puncture (aka spinal tap). Now this study is not about me and normally (and hopefully) I don't get any feedback. However, they assure us that if they do find anything of concern they'll let me know and then I would need to get my own medical evaluation. So that MRI and spinal tap happened in October and I got any feedback which I'm taking as a good sign.

 But it doesn't mean I'm clear. If you've heard about the plagues and tangles associated with
Alzheimer's there is considerable controversy
whether they themselves are the cause or the result of Alzheimer's. There is now a lot of evidence that they don't cause the disease, but a
body reaction to it and specifically a defense. The problem is not everyone with Alzheimer's has the plaques, and some people who have the
plaque do not get Alzheimer's. But, obviously, if they do find them it's very concerning.
Since so far I haven't got any feedback from the study so
I'm taking that as good news.
But it doesn't mean I'm clear. If you've heard about the plagues and tangles associated with
Alzheimer's there is considerable controversy
whether they themselves are the cause or the result of Alzheimer's. There is now a lot of evidence that they don't cause the disease, but a
body reaction to it and specifically a defense. The problem is not everyone with Alzheimer's has the plaques, and some people who have the
plaque do not get Alzheimer's. But, obviously, if they do find them it's very concerning.
Since so far I haven't got any feedback from the study so
I'm taking that as good news.
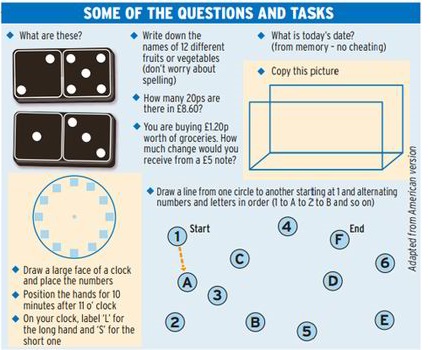 The visits for the Alzheimer's study are a combination of mental and physical exams. The mental part is answering questions and
reciting back lists that they read you.
The visits for the Alzheimer's study are a combination of mental and physical exams. The mental part is answering questions and
reciting back lists that they read you.
The physical exam is in two parts. When you arrive they take blood samples that get analyzed very quickly and after the cognitive testing you meet with a nurse who then does a physical exam and then goes over the blood tests which this nurse had on a piece of paper. This was my second Alzheimer's test and had these same ones run a year previous. I didn't take any stock in them the year before, but I noticed that one of the screens was a CRP, one of the two tests for inflammation. I was astounded by the reading, 3.7, as I remembered that number was 10.9 in early June. I was doing a lot better, but was wondering if it was a simple case of getting used to the pain. This was a real indication I was doing better and it was just two and a half months later! The following week I had an appointment with a rheumatologist that I was actually thinking I should cancel because I already had a diagnosis and I was already getting better. But I decided I really wanted to know for sure and to see if there was anything the rheumatologist could recommend.
Rheumatologist
On August 27th I had my appointment with Rheumatologist Dr. Judy Goldstein. Going in I thought this was going to be short and sweet, simply getting confirmation of the Polymyalgia Rheumatica (PMA). But before that she went through the history with the high inflammation markers and the near elimination of the symptoms by the short presciption of prednisone. But then I informed her of how I was doing now and said I felt I was doing much better and then offered what I had learned from the Alzheimer's visit: my CRP reading was down to 3.7 from the 10.9 in early June. This got her attention! She said she would have me visit the lab for a blood test for a current ESR which was 26 back in June. Dr. Goldstein finally concluded with something I never expected. She said had she seen me in May she would have agreed with the diagnosis of PMR, but says there's no way it can be PMR because of my improvement. She stated "No one starts to get better from PMR in under a year." I protested because I'm in really good shape, but she repeated herself, "No one gets better in under a year."
The lower inflammation was further confirmed as the new ESR was an amazingly low 6, with a std range of 0-15 when it was 26 a few months earlier. Thinking of the improvement of the other inflammation test, the CRP going from 10.9 to 3.7 made me go back to the physical exam I had for the Alzheimer's study the year before. Sure enough there was the CRP but it was at an incredibly low 0.4! That was an indication my inflammation level had a lot further to fall.
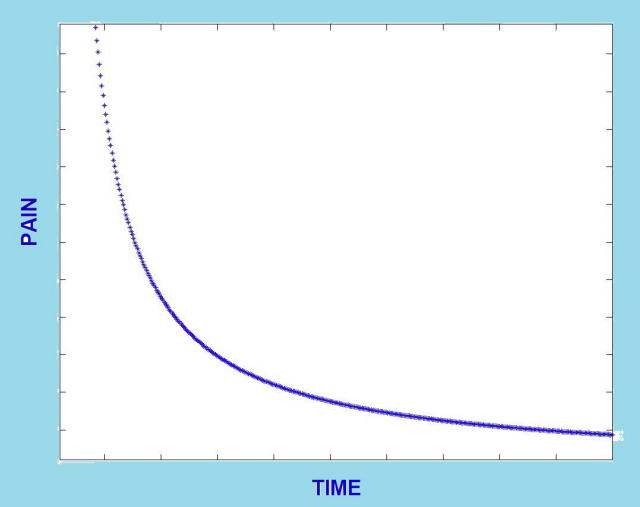 So to this day I don't know what it is, but it continued to get better, but at a reduced rate. I thought it would be mostly gone by November, then December,
then by a year, but the improvement was only gradually better. In retrospect my improvement seemed to follow an
asymptotic curve: very quick at the beginning with gradual decline over
time.
You would think someone might be interested
in my case because I keep thinking, "What if I really do have PMR? What is it about me that is different? Might they not learn what it is so it
can help others with PMR?"
So to this day I don't know what it is, but it continued to get better, but at a reduced rate. I thought it would be mostly gone by November, then December,
then by a year, but the improvement was only gradually better. In retrospect my improvement seemed to follow an
asymptotic curve: very quick at the beginning with gradual decline over
time.
You would think someone might be interested
in my case because I keep thinking, "What if I really do have PMR? What is it about me that is different? Might they not learn what it is so it
can help others with PMR?"
Continue to The Road to the Confirmation of Cancer
