Prostate Cancer
A Lifetime of Good Health Ends
The Road to the Confirmation of Cancer
 I got scheduled for the prostate biopsy which would be performed by Dr. Schlesinger. The worst part of this was I had to be off of the ibuprofen
for 7 days before the procedure. I then found out how dependent
I was on them to keep the pain down. The other part was the biopsy required that I give myself an
enema before coming for the appointment.
The procedure itself was fine without any real pain and the first thing she did was measure the prostate and said, "Hmmm... your prostate size
seems normal" with the sound of surprise in her voice. I had to ask, "Is that a good thing?" and she said yes.*
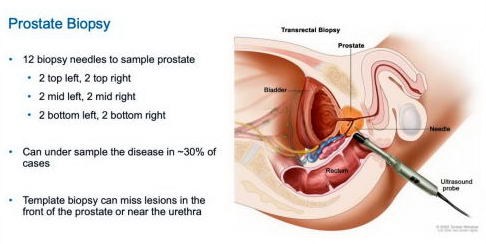
She took 12 samples, 6 on either side of the prostate. Every time a sample was taken you could
hear a very audible click. She said that though
the results of the biopsy would appear in a few days on the MyChart, don't look at them. There will be a follow up visit 7 days later when
she'll go over everything. I complied with her wishes and then she was surprised that I didn't look.
I got scheduled for the prostate biopsy which would be performed by Dr. Schlesinger. The worst part of this was I had to be off of the ibuprofen
for 7 days before the procedure. I then found out how dependent
I was on them to keep the pain down. The other part was the biopsy required that I give myself an
enema before coming for the appointment.
The procedure itself was fine without any real pain and the first thing she did was measure the prostate and said, "Hmmm... your prostate size
seems normal" with the sound of surprise in her voice. I had to ask, "Is that a good thing?" and she said yes.*
She took 12 samples, 6 on either side of the prostate. Every time a sample was taken you could
hear a very audible click. She said that though
the results of the biopsy would appear in a few days on the MyChart, don't look at them. There will be a follow up visit 7 days later when
she'll go over everything. I complied with her wishes and then she was surprised that I didn't look.
* In my later research this was not good, this was decidedly bad. An enlarged prostate raises your PSA so that could explain all of the elevation. So the fact it was so high without an enlarged prostate meant there probably was cancer. I think the doctor was caught off guard with my question and didn't want to immediately give me bad news at that moment.
"We didn't find any cancer."
In the follow up appointment to discuss the biopsy results it started out encouraging as she walked into the room, "We didn't find any cancer," which was obviously great news, but we were soon deflated. The result was not totally conclusive. One side of the prostate was definitely good, but there was some signs it might not be on the other side. The sad fact is there a huge constraint on a biopsy such as this which is where do you look? The urologist only takes 12 samples (6 from one side, 6 on the other) and it's simply a hit or miss. If one of the samples is positive, you get the confirmation there is in fact cancer, but you don't know how extensive. But if it's a small area it's easily missed. She didn't say, but I think a big reason for her opinion was the high PSA with a normal size prostate.

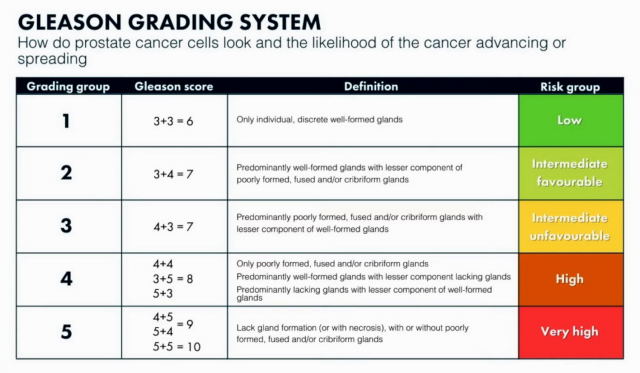
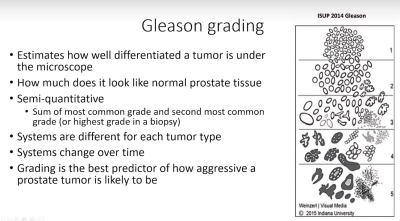
A week later I had a video appointment with Dr. Schlesinger to go over the results of the biopsy and the next steps. The results definitely confirmed the MRI that it was cancerous and exactly what the MRI showed. In technical terms, it's Prostatic Adenocarinoma, Gleason score: 4+3=7, Grade Group: 3". Translation: Unfavorable Intermediate risk. Therefore, active surveillance was not a possibility. Her strong recommendation was for the prostate to be removed because of my age and good health. I asked if I could wait until March because I would then be on Medicare, but she strongly recommended this be done ASAP. She did mention that an option was radiation, but in her opinion surgery should be the way to go. Now I would have thought this could be a simple matter of removing the tumor, but instead they would remove the entire prostate! She didn't explain why, but my research showed that they want to eliminate not just the tumor, but any possibility that new cancer cells are formed. The downsize, however, is obvious: you lose your prostate which may result in no sexual function and the possibility of incontinence so I might be wearing a diaper for the rest of my life. She also said something I never forgot: If you ask a surgeon for their recommendation, they're going to say surgery. If you ask a radiation oncologist, they're going to recommend radiation.
So now I officially have prostate cancer and I got a video appointment with Dr. Robert Bloomberg who would be the surgeon as this is who Schlesinger recommended. He didn't go into any real detail about the procedure other than it was "robotic" and would take 4 to 5 hours. I would have to look up the advantages of this versus standard surgery. Technically, it's called robot-assisted surgery, and it's the newest technology. Compared to standard surgery, it's better at getting out the entire prostate and at the same time saving as much of the nerves as possible. If enough nerves are saved, sexual function is not lost. Finally, your recovery time is faster. But he didn't mention the incontinence issue and he didn't really inspire any confidence and what really disappointed Debbie was that he didn't tout his experience like "I've done hundreds of these." We finished the video call without really making next steps which would be getting back to his staff to get onto the schedule. We were warned that it can take 10 days to get on the schedule and the stated reason was time on the "robot" is very limited.

Though I had already made a tentative decision that I'd get the surgery, I also got a referral to a radiation oncologist to investigate that option, especially because it just sounded easier and the best part is I'd get to keep my prostate. I met with Dr. Thomas Lambert and it really wasn't easier. He described a 9 week treatment regimen 5 times a week. The treatments would start off okay, but you'd get increasingly tired as they went on and essentially the radiation would be burning you up inside. A description I read later described the process as "turning the prostate into a lump of coal." On top of that there would be a number of visits for preparation and he really didn't say (and I didn't ask) how long it would be until I got a schedule. In retrospect, he didn't really tout that there was less risk of the loss of sexual function and that incontinence was rarely a problem. Without that information, the recommendation to get the surgery now seemed to be the correct one. But as Dr. had warned, he did recommend radiation.
In retrospect, this consultation was practically a joke as he only offered one treatment regime. No brachytherapy, no 4-week option, no mention of SBRT (which can often be done with just 5 treatments) . I don't know if it was the doctor, but my suspicion it had more to do with my insurance. But if that's the case, why wouldn't 4-week be an option as it has to be less expensive then 9-weeks? Also in retrospective, I needed to do a lot of investigation before so I could have asked these questions.
ASAP - January 13th!
So now I needed to get on the surgery schedule. But unfortunately just getting scheduled for surgery takes a long time because time on the robot is limited. I was told it can take 10 days just to get on the schedule! I got on it in just 7 days so I was supposed to be grateful for that. Then the earliest date available for the surgery was January 13th! Really? This is some new definition of ASAP. So with that scheduled we decided we might as well head to Arizona, now just a week late from our usual departure. Our route would first take us through Des Moines and then south to Kansas City where we would stay the night and the following morning have breakfast with Debbie's cousins, Linda and Cathy, who both live outside of the city. Then it was south through Wichita and then the pan handles of Oklahoma and Texas staying our final night in Santa Rosa, NM. From there I-40 west to Flagstaff and then I-17 down to Phoenix. But once again the route through Kansas and the pan handles was so boring and is so riddled with state patrol cars waiting for speeders we vowed to take an alternative in the future.
We would have to be back, however, by Christmas because you need to get a complete physical about 3 weeks out from the surgery. The reason so early is in case something is discovered and then requires another appointment or 2. My date was December 21st. Then 10 days out you have to get a set of labs which involves blood tests and a urine sample. Finally, 3 days out you need a COVID test.
A Special Prayer Shawl
Debbie is part of a Prayer Shawl ministry so she knits/crohets prayer shawls that when complete are blessed by a priest and then given to someone with a health problem. Normally these are just turned into the ministry and given out as needed. Only occasionally does she pick the person. She's done exactly 82 of them so far, but number 82 is special because she knit it for me!

Above is the completed Monarch Butterfly prayer shawl.
Click here to read the story plus more pictures.
Return For Surgery
Everything at this point should be on autopilot. No such luck. Fasten your seat beats! It's going to be a ride and specifically, a roller coaster ride.
The drive back to WI takes us 3 days because we can only drive so far with the cats, and Debbie prefers we don't drive more than 10 hours any day. So we loaded up the van and took off on December 18th. On the first day we stopped in Santa Rosa, NM, and the second day in Joplin, MO. We were on the 3rd day a few hours from St. Louis when we get a call that the surgery with Dr. Bloomberg had been canceled due to "a scheduling conflict" which was never adequately explained and our urologist suggested it was a staffing issue which is a euphemism for incompetence. But remember the 10 days? Suddenly right in the middle of the phone call where they canceled they were able to reschedule the date on the spot which was February 17th. The really irritating part was it was now too late and we were committed to continuing on for the 6 more hours until we reached WI, had we known 2 days earlier we could have stayed in AZ for another month! So now we'd just have to wait another month for the surgery and given a minimum of 6 weeks of recovery, it might be impractical to get back to AZ this Spring.
Obviously I was disappointed, but Debbie was angry because she didn't trust that surgeon in the first place. We asked Dr. Schlesinger if there was another surgeon and she suggested Dr. Fred Banks. Banks at first was incredulous as the best date he had was February 15th, but Dr. Schlesinger informed him exactly what had occurred and agreed to take me for the date in February. We had a video call with him and I was pleased that he seemed to be better than Dr. Bloomberg.
This was our first winter together in Lake Mills since from 2016 we've spent this time in Arizona. We've been back for a brief time around Christmas, but it was mostly spent visiting family and the Christmas activities. The highlight was being able to go to the Lake Mills Knickerbocker Ice Festival which was held on Feb. 3rd and 4th. The highlights are shown in the pictures below.
Ever since the first surgery date got canceled I'd lived with the fear that something was going to stop this surgery from happening again. Consequently it was up to me (with considerable assistance from Debbie) to stay healthy and be sure nothing gets in the way. I felt it was fine to do outdoor activities. And everything was going fine coming into the surgery. I passed my physical done by PA Lucy Whitman (no issues), lab tests (nothing), and COVID (negative). And seven days before you are off any medications and for me the big one is no ibuprofen. I was ready! And I was so ready for this whole thing to be over!!
Continue to Surgery