Prostate Cancer
A Lifetime of Good Health Ends
Surgery!
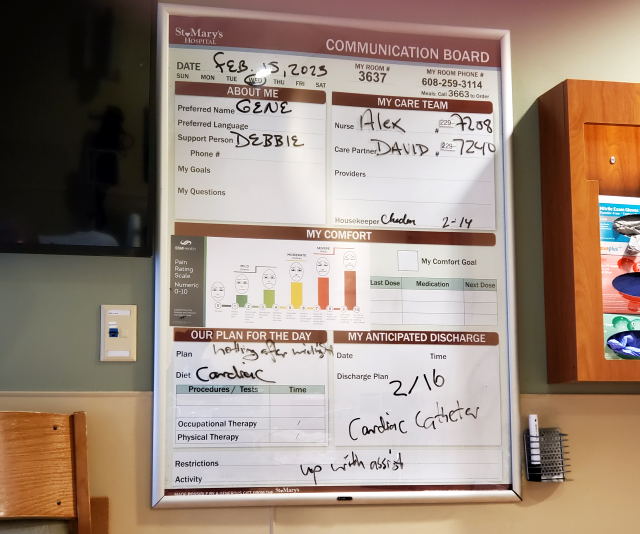
On February 14th, the day before the surgery, I had to stop eating most solid foods 24 hours before the surgery start time (8:00AM), then switch to only soft foods, and then finally, only clear liquids. I also had to drink an enema. On the morning of February 15th I was up by 4:30AM because I needed to take a thorough shower and then apply a special disinfectant soap, especially around "the surgical area." They never actually said specifically where that was so I was guessing. They then say you need to come in clean clothes and underwear, which you would think would be a no brainer, but they're obviously in the instructions because of past cases when this was not done. A change of clothes was also needed because I would have to stay in the hospital overnight to be sure I was having a satisfactory recovery. I had no breakfast as you needed to be fastening for the surgery and me and Debbie took off to St. Mary's Hospital in Madison at 5:25AM for the specified 6:00 arrival.
We arrived right on time in the dark and I was frankly quite excited that the day had come and soon this would all be over. At least the surgery part as I was not thinking of the possible post surgery urination difficulties and loss of sexual function. There was a quick check in and you were official when they put on the wrist identification band. If all went according to plan I'd stay overnight and then released the following day. Staying overnight was the only thing that I didn't like, but I knew they needed to be sure I was recovering.
I met first with a nurse who would do all the initial prep. He was very friendly and I was in a really good mood. At the end I made a joke, "Are you sure you marked the correct prostate for removal?" Judging from his laugh he apparently never had a patient joke about that before. If you're not aware, from some cases of kidney removal the surgeon took out the wrong one! Now they always are sure to double check and mark the correct one. Of course men only have only one prostate, a situation that will be changed after the surgery when the number would be zero.
I then met the anesthesiologist, Dr. William Sherman, who asked me if I had any questions and I don't think he expects any real questions. But I feel I should inform him of the last (and only) time I went under general anesthesia where it took a very long time to recover. He responded with a simple, "That won't be a problem." He made no mention that he was already aware of this, but his notes after the fact shows he would only use moderate anesthesia based on previous medical history. I thought about joking about "My life is in your hands," but that's not a joke because that is in fact the case! The meeting with Dr. Sherman ended with him giving me the shot that would put me out and they immediately rolled me into the operating room. When he gave me the shot he gave me no warning about what was going to happen, but I was already prepared to be almost instantly in the recovery room as that's how general anesthesia works. You don't dream so no time seems to go by so for me the 4-5 hours would go by instantly.
"I think it was an MI!"
I would awake immediately, but to a surreal scene as I can tell I'm in the operating room! It's confusing because it looks like they're closing down, but I know something went wrong. I then hear a voice from behind me say very loudly and clearly, "I think it was an MI!" Even in my groggy state I knew exactly what that was. A Myocardial Infarction or Ischemia, i.e., a heart attack. I surmised it was my anesthesiologist and clearly, he didn't know at that point I was conscious or would have never uttered those words out loud. I was just confused, but I knew why the operation was terminated. How could I have a heart problem? Apparently they didn't get very far and the anesthesiologist shut it down as the EKG showed two bad anomalies and he suspected I might be about to or were having a heart attack.
Post Surgery - 30 Hours of Hell
At that point, however, I couldn't process it and was just confused. Heart attack? I was in mental paralysis and really couldn't even think of anything I should ask. I got wheeled out to a holding area where they said they needed to do an EKG and draw some blood, not telling me what they were testing nor why all this was going on. But because I had heard what the anesthesiologist said, everything they did made perfect sense so I didn't feel I needed to ask any questions. They kept asking me how I felt. Any chest pains? Any tingling in the fingers? I knew the blood was to test for the enzyme that will be almost 100% conclusive that a heart attack had or had not occurred. The question about any chest pains would be repeated a lot over the next 30 hours and I would eventually feel I should have a recorded message that I could call up by the push of a button. "No I don't have any chest pains. I've never had chest pains!"
Sadly, I was so self-absorbed at that point I didn't think at all about Debbie who was in the waiting room expecting a 4-5 hour procedure. She was approached by a staff person, but Debbie said they couldn't want her as my surgery wouldn't end for many more hours. But, no, it was her they wanted. She then got scared half to death thinking the worst when the surgeon, Dr. Banks, came in to tell her there was there was an anomaly in the EKG and they had to shutdown the procedure. He then tells her I was being examined by the cardiologists and if they give their clearance, the operation will occur the following day. In retrospect, I don't see how that would have ever happened. He didn't mention a possible heart attack.
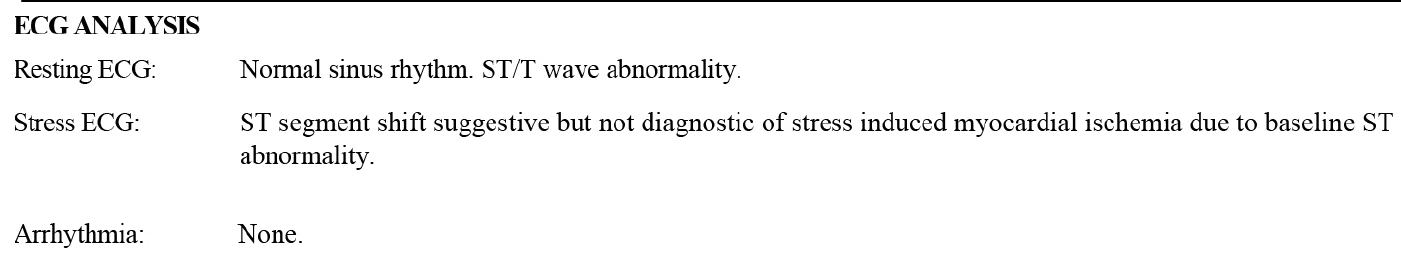
 At the left is a schematic of a single cycle of a heart beat on an EKG/ECG with the segments identified. There will be mentions of the ST segment and the T wave
in this coming section as it's all about the heart.
At the left is a schematic of a single cycle of a heart beat on an EKG/ECG with the segments identified. There will be mentions of the ST segment and the T wave
in this coming section as it's all about the heart.
After the fact the surgeon, Dr. Banks wrote in his report: "Shortly after establishing pneumoperitoneum and performing diagnostic laparoscopy, he developed ST changes, which were persistent concerning for cardiac ischemia. Given his history of aortic stenosis [heart murmur], it was felt unsafe to continue the operation for fear of creating a significant cardiac ischemic event and so the procedure was ended." I need to mention this was written much later as it doesn't match with the anesthesiologist who thought it was in fact a cardiac ischemic event.
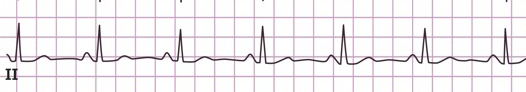
Normal ECG segment II. Click/tap on the image to see all the leads.
My ECG segment II during the surgery that might imply myocardial ischemia, but it looks weird. Click/tap on the image to see all the leads.
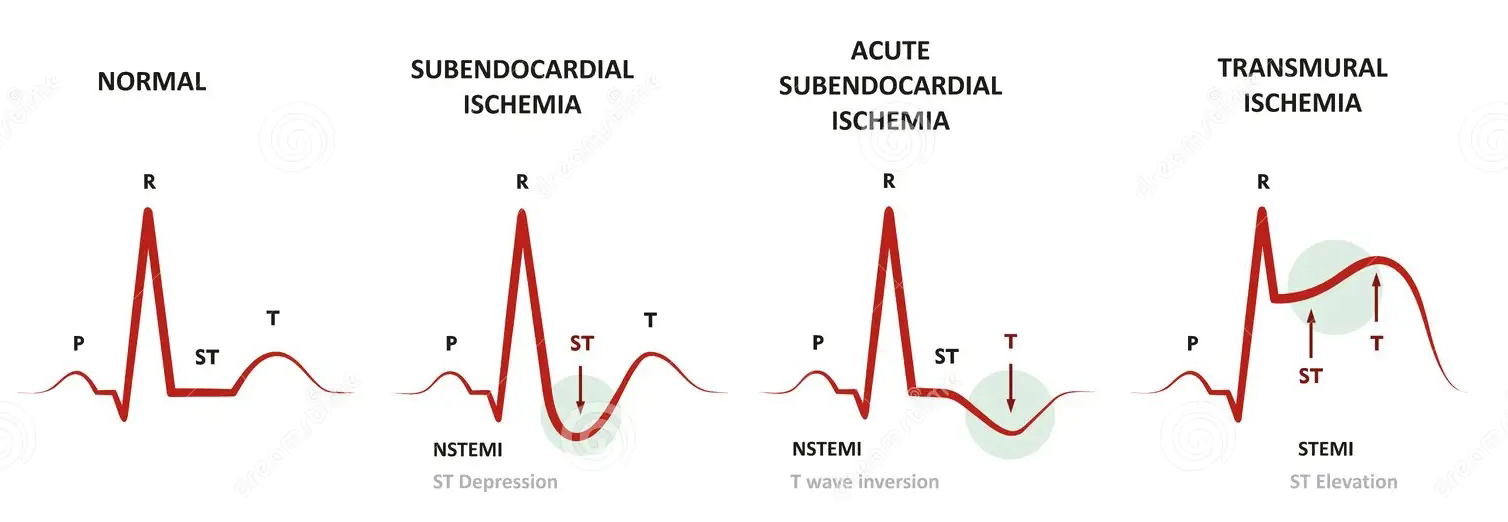
Types of ischemia with normal reference. My ECG indicates an ST depression meaning Endosubcardial Ischemia.
Troponin Test Result: "No results for input(s): TROPONINI, TROPONINT, TROPONIN in the last 87600 hours." So no heart attack evidence over the last 10 years.
80% Chance
But by the time I was rolled into my hospital room (not in the cardiac wing because a room was not available) they knew that there was no heart attack because the three blood tests for troponin were negative. Also, the EKG was normal just as it was before the surgery. But there is an issue with being assigned a team of cardiologists. There's an expression that goes, "If your only tool is a hammer, then everything starts to look like a nail." So ... if you get a cardiologist, everything looks like heart disease, and in this case it was looking like one very large nail! The spokesperson for the group was Dr. David Nguyen, who I would get to know very well. He was very personable and was born in Vietnam He didn't waste a lot of time to start preparing me for the worst. The small glimmer of hope was I had maybe a 20% chance it would be nothing. But he then went on to the depressing stats. There was a 70% chance that there is a blockage that will have to be immediately addressed, and never mentioned the remaining 10% which would be really bad: a blockage so severe it would require bypass surgery. Doing the simple math, there was a 80% chance I had bad coronary heart disease, a probability that was depressing. In retrospect I was a little annoyed that he didn't inquire about either my personal health and especially about my physical conditioning. Nguyen also warned me that it might be difficult getting the surgery because they might not be able to find a willing anesthesiologist. This statement will haunt me later.
Dr. Nguyen's comment in his report: "During surgery preparation and sedation, he was found to have ST changes on telemetry strips including ST elevation in leads V5 and aVL and ST depression in lead III. He is extremely active at baseline without cardiac symptoms. He has known mild aortic valve stenosis." Curiously, at the top of the ECG a cardiologist does not mention ST, but rather a "Nonspecific T Wave Abnormality."
I completely forgot that as part of the surgery they'd insert a Foley catheter and then removed it when the surgery was aborted. It would have remained inserted if the surgery had been successful. But I was painfully reminded when I needed to urinate. Getting started was extremely difficult and fell back to difficult when I finally got a flow started. I would dread every time I needed to go and I would need to drag the IV along with me and struggle to get the tube out of the way. Fortunately, every trip to the bathroom became ever so gradually easier. Another thing that was irritating was I wasn't permitted to eat because Dr. Nguyen thought I could get into surgery immediately once they ran their tests.
 That afternoon I got a
nuclear stress test
that I thought went well, although I endured a series of, "Are you
feeling any pain? Any chest pains? How do your arms feel?" Negative,
negative, negative. During the procedure I could see Dr. Nguyen who was
monitoring the procedure through the window and he didn't look happy and
to me it was an ominous sign. I didn't have to wait very long for the
results, and it was a little damning in that it
suggested a blockage, an area my cardiologist called "an area of concern." In the notes they also said, "Abnormal Stress Test."
That afternoon I got a
nuclear stress test
that I thought went well, although I endured a series of, "Are you
feeling any pain? Any chest pains? How do your arms feel?" Negative,
negative, negative. During the procedure I could see Dr. Nguyen who was
monitoring the procedure through the window and he didn't look happy and
to me it was an ominous sign. I didn't have to wait very long for the
results, and it was a little damning in that it
suggested a blockage, an area my cardiologist called "an area of concern." In the notes they also said, "Abnormal Stress Test."
However, a reading of the stress test report by an independent cardiologist (which I would not read until months later) gave me insight that the situation was not clear cut. My assumpton is that cardiologist had no background knowledge as to why they were doing the stress test so for that doctor it was a blind evaluation.
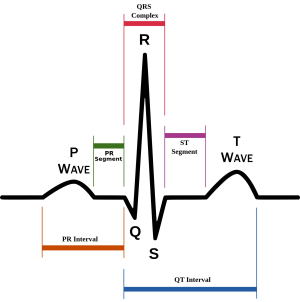
I would be told a couple of times that I had a normal EKG/ECG outside of what happened in surgery, and the report clearly says "Normal sinus rhythm, but then it says I have ST/T wave adnormality at rest. And the doctor then notes the ST shift is suggestive, but not conclusive of myocardial ischemia. My reading is this is an oxymoron. But reading up on ST/T wave abnomrality is that this is what they call a "non-specific" anomaly so not indicative of any real problem.
Dr. Nguyen informed me soon after the test they'd have to do a heart catheterization which he described as the "gold standard" in determining heart disease. I can't put my finger on it, but the way he phrased it along with other comments led me to believe they really wanted to do the procedure regardless. But part of this to me was hardly a surprise since ECG/EKGs often are misleading because of false positives and false negatives. Unfortunately, the catheterization would occur the following day so I would have to endure nearly 24 more hours of what was now looking like certain heart disease as they'd apparently found something significant. My life as I knew it was now over. I have a permanent issue with my heart and would therefore have to be extremely careful in everything I did going forward as this could kill me. And because I've obviously lived with this problem without feeling one iota of chest pains, I would not get any warning. So I would not only have to be careful, I might not be able to do anything resembling significant exercise for the rest of my life.
 I was already going to stay overnight in the hospital because of the
prostate surgery, but if they couldn't do the catheterization early enough, I would have to stay another night. The first night wasn't really too
bad because I wasn't in the cardio section so the nurses didn't demand anything, and the fasting
regime that had started 24 hours before the surgery ended when I was permitted to order a meal as any surgery would be more than 24 hours later.
The prostate cancer itself, however, now seemed so trivial.
I was already going to stay overnight in the hospital because of the
prostate surgery, but if they couldn't do the catheterization early enough, I would have to stay another night. The first night wasn't really too
bad because I wasn't in the cardio section so the nurses didn't demand anything, and the fasting
regime that had started 24 hours before the surgery ended when I was permitted to order a meal as any surgery would be more than 24 hours later.
The prostate cancer itself, however, now seemed so trivial.
Overnight I had time to contemplate everything alone as Debbie was not staying there.
After she got home she texted me the picture on the right. Our cat Portia who is definitely my cat will always stick around
the door as Debbie generally enters the house before I do. So to Portia, Debbie entering means I will soon follow.
Debbie's text said, "She's missing you!"

My thoughts lead me to only one conclusion which was I'm in uncharted territory. I'm the oldest living male member of my immediate family. My dad died at age 60. My older brother, Erik, died at age 57. My dad's dad (my grandfather) died at age 50. All three died because of alcohol abuse. So it was possible there is a genetic problem and heart disease does run in the family. So far no trouble with my younger brother of 2 years, and my sister as well, although Alzheimer's has essentially already ended her life as she is now in permanent memory care. My mom had a weird valve issue that they thought was serious as was indicated by several EKGs, but actually turned out to be trivial after a heart catherterzation was performed which indicated that the problem was minor so no necessity of a heart valve replacement.
90% Chance
Late in the morning the following day I got a visit from Dr. Charles Jones who would be performing the catheterization and he was hardly a ray of sunshine. He put everything in stark terms and exuded the impression that he never smiled or otherwise ever had a happy thought. And he had new probability stats: There's a small possibility they would find essentially nothing. He gave the probability at just 10%. Very memorable to me because the day before Dr. Nguyen pegged it at 20%. He then said there is an 80% chance they'll find a significant blockage and if they do, they'll open the artery with an angioplasty (a balloon) and then insert a stent to keep the artery open. I was already well aware of the procedure. Then he went there: a 10% chance they'll find a blockage so severe it can't be cleared so that I would need heart bypass surgery. He informed me the procedure generally lasts an hour if they put in a stent, but longer if they find several issues. He didn't add any words of encouragement. He was a quintessential example of a medical specialist: great at treating diseases, but utterly incompetent in treating a patient. I would find out much later by looking at his notes that he felt I was at high risk for myocardial ischemia. To him putting in a stent was a slam dunk and he needed to set my expectations accordingly. The chances that there was really nothing or essentially nothing there were almost nil. Yes, it was now confirmed that my life as I knew it was over.
"What the hell is going on here? This makes no sense!"
An hour or two later my GP, Dr. Smith, unexpectedly makes a visit. I wasn't even aware he knew about my prostate surgery. He walks into the room and he's a little indignant. "What the hell is going on here?" An entirely rhetorical question as he knew exactly what was going on as he had just read all the charts. So not waiting for an answer, he then says, "This makes no sense! How can you have a heart problem?" He goes on to list all the reasons: the EKG looks good, my physical conditioning, not overweight, good cholesterol, don't smoke, don't drink, etc. etc. I got my first actual piece of information that made me feel better, if at least for a while. It was his opinion that there was no real heart problem. I simply had a bad reaction to the anesthesia. Sadly, I didn't give what he said any real credance. How could my lowly GP know better than a team of cardiologists who were currently examining me? And, really, maybe he didn't read the nuclear stress test results which I was lead to believe were pretty damning.
"It all looks good. Nothing we need to do."
 At 2:45PM I got taken to the catheterization lab. Debbie would be waiting
in a room near the procedure where she would get word when it was over. It
was maybe 10 minutes of prep, getting the needle through my right wrist
which seemed effortless. That's the preferred path to the heart. If that doesn't
work they then have to go through your right leg. I really felt no
discomfort, but it did feel more than a little warm when they injected the
contrast dye. Dr. Jones then came in and simply asked me how I was doing
and I said, "I'm good!" The actual procedure then started and he said nothing and for a
few moments here and there I could see the 70+ inch screen showing the
inside of my arteries which I found fascinating and for a little bit I forgot how serious the situation was.
But it was all done in what seemed like less than 5 minutes by Jones just saying, "It all looks good.
Nothing we need to do." I was frankly in shock, not believing what I had just heard.
Of course, he didn't didn't say anything to me like, "Gene, that's great news." He just left.
It was another 5 minutes of post procedure and
I was wheeled out. Basically, if I'm giving the cardiologists the maximum benefit of the doubt this was about
1) liability and 2) insurance.
They always want to do the catheterization because it's so decisive. But they have to be able to justify it.
At 2:45PM I got taken to the catheterization lab. Debbie would be waiting
in a room near the procedure where she would get word when it was over. It
was maybe 10 minutes of prep, getting the needle through my right wrist
which seemed effortless. That's the preferred path to the heart. If that doesn't
work they then have to go through your right leg. I really felt no
discomfort, but it did feel more than a little warm when they injected the
contrast dye. Dr. Jones then came in and simply asked me how I was doing
and I said, "I'm good!" The actual procedure then started and he said nothing and for a
few moments here and there I could see the 70+ inch screen showing the
inside of my arteries which I found fascinating and for a little bit I forgot how serious the situation was.
But it was all done in what seemed like less than 5 minutes by Jones just saying, "It all looks good.
Nothing we need to do." I was frankly in shock, not believing what I had just heard.
Of course, he didn't didn't say anything to me like, "Gene, that's great news." He just left.
It was another 5 minutes of post procedure and
I was wheeled out. Basically, if I'm giving the cardiologists the maximum benefit of the doubt this was about
1) liability and 2) insurance.
They always want to do the catheterization because it's so decisive. But they have to be able to justify it.
Some images from the heart catheterization given to me by Dr. Nguyen. To my untrained eye, I don't see any blockages.
Debbie was once again waiting expecting the procedure to take an hour or more (so we were told) and thought the worst when they came to get her so soon. But all they said was, "He's good. They didn't find anything."
Against the odds
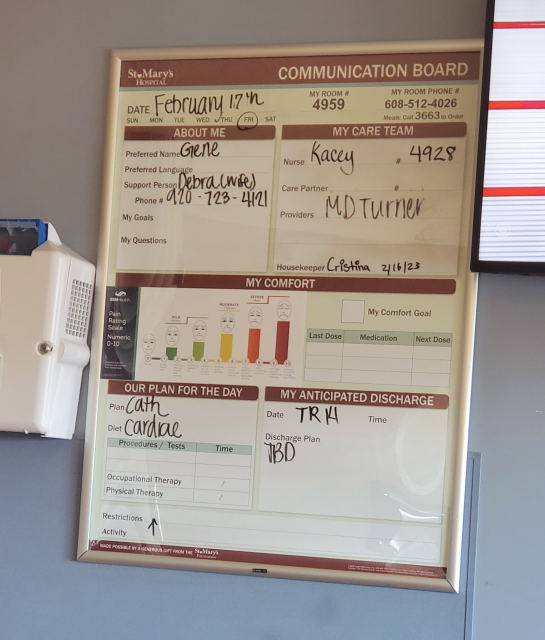 After the catheterization I was wheeled to a new room, this time in the cardiac ward. I was soon joined by Debbie and when it was just me and her,
I was suddenly so overcome with emotion because of what had just happened I just started to cry. Against the odds I didn't have the serious heart problem they were so
certain I had. Debbie was concerned and asked what was wrong. I let her know
I was happy and so relieved that the nightmare was over. To me it felt
like I was one of those unlikely survivors of some catastrophe that kills everyone around them, but somehow they're saved.
This is not that they didn't find anything, but what they found was very trivial and is considered
very good for someone my age according to my GP, Dr. Smith.
After the catheterization I was wheeled to a new room, this time in the cardiac ward. I was soon joined by Debbie and when it was just me and her,
I was suddenly so overcome with emotion because of what had just happened I just started to cry. Against the odds I didn't have the serious heart problem they were so
certain I had. Debbie was concerned and asked what was wrong. I let her know
I was happy and so relieved that the nightmare was over. To me it felt
like I was one of those unlikely survivors of some catastrophe that kills everyone around them, but somehow they're saved.
This is not that they didn't find anything, but what they found was very trivial and is considered
very good for someone my age according to my GP, Dr. Smith.
So obviously great news. It is an anomaly and any explanation for what happened during the surgery we may never know, but the only explanation that seems credible is a reaction to the anesthesia. And remember I told you earlier to fasten your seat belt. It turns out we were just on a roller coaster ride and you know what happens in the end: you wind up exactly where you started.
Before all this happened, I knew two major problems with our current health system is that so much of it is driven by the avoidance of liability and the providers navigating insurance. So you should expect that they sometimes do the inexplicable. I also learned the limitations of specialists. I wrote before "If your only tool ..." problem with the cardiologists, but I feel another problem is that they may be good at treating a disease (after all, they're specialists), they can be very poor at treating a patient.
I was still technically fasting because Dr. Nguyen was still sure I'd get the surgery immediately. I didn't tell him I thought that was never going to happen. The attending nurses in this ward were especially friendly and appreciated a little levity. I don't think they're used to getting many patients like myself that have gone through a heart catheterization with nothing performed. Every 8 hours you get a shift change with one nurse and/or assistant saying goodbye and then a new nurse and/or assistant coming in to greet you. The instructions were always, "Let us know if you need anything and let us know immediately if you feel any pain." Then hours later they'd ask if you're feeling any pain. By the third time I couldn't help but be sarcastic. "You told me I was supposed to immediately let you know. So that is a trick question!" The nurse laughed at that. Really the only thing that needed be be checked was my wrist wound from the catheterzation. I had a dressing that needed be changed and I wore a wrist restraint.
Though I could have probably gone home as Dr. Nguyen had officially given the cardiologist release for surgery, Debbie had come planning on staying the night and we had a lot of snow with more threatening, making driving unsafe. She would spend the night with me. I had the comfortable bed and she had the very uncomfortable couch. The following morning (now February 17th) we got the official release and headed home, never hearing from Dr. Banks or anyone from his staff. You'd think I'd get a new surgery date right away, but it was the following Tuesday and the date was April 12th. I asked what the next date would be and it was May 4th so I took that one. Of course I was thinking of the extra time we'd get in AZ. I'd get a call a week later that Dr. Tierney thought I should get the surgery earlier, but the whole concept of ASAP had been thrown out the window by that time. As I thought about it over time I was increasingly bothered by what Dr. Nguyen had said about finding it hard to find a willing anesthesiologist given the ECG/EKG. I would think I would get a consultation with the staff of anesthesiologists about another surgery for their opinion. But there was nothing and so with that once again we decide we should go to AZ for 7 weeks.
Back to Arizona
At that point we had made 7 round trips to Arizona so it's become a routine and usually uneventful resulting in an unmemorable experience. Our trip to AZ in October of 2021 was memorable because of our newly adopted cat, Portia. She had come out of the woods just 16 days prior and for the first 10 days we weren't even sure we could keep it. This was her first long car ride and our fear was that she would go berserk and we'd need to just let her go and then how'd she do in a hotel room with the other cats. But in the end what was memorable was how anti-climatic it was. She's a better traveler than the other two cats and did great in the hotel rooms. Weather is always a concern so we normally plan accordingly. We're not on a strict schedule so we have the luxary of choosing when we leave to avoid bad weather. In October of 2019 we stayed in Denver too long and during the evening a big snow storm hit. We left late in the morning, but we mostly drove through snow and ice covered roads, seeing many cars that had slid off the road.
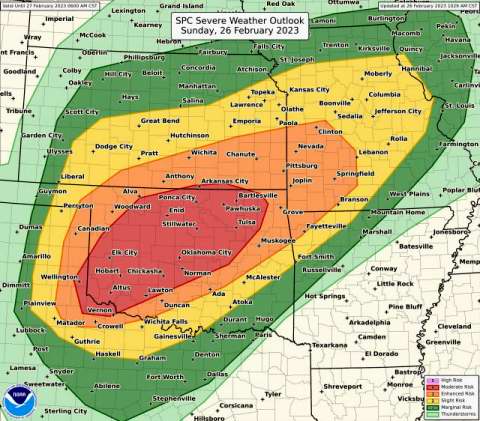 This time I chose the most southern route because it was the middle of February and it all started great.
We stayed the first night in Joplin, Missouri, at a LaQuinta which we
stayed at on the way to WI. Then on the second day after driving through
Oklahoma we got to Texas and then, just outside of
Amarillo, we hit a
derecho
that slowed us to a crawl. Fierce winds and blowing dust with visibility
as little as 50 feet at some points. We encountered two accidents and a field fire. I was okay with the
drive in those horrendous conditions because I had experience driving
through the monsoon dust storms around Phoenix. We were so happy to get to
the New Mexico sign as shortly after we were through the storm. This storm made the
List of Derechos on Wikipedia and
has its own
page for the one we drove through.
What was most frightening is that we missed the main part of the storm!
This time I chose the most southern route because it was the middle of February and it all started great.
We stayed the first night in Joplin, Missouri, at a LaQuinta which we
stayed at on the way to WI. Then on the second day after driving through
Oklahoma we got to Texas and then, just outside of
Amarillo, we hit a
derecho
that slowed us to a crawl. Fierce winds and blowing dust with visibility
as little as 50 feet at some points. We encountered two accidents and a field fire. I was okay with the
drive in those horrendous conditions because I had experience driving
through the monsoon dust storms around Phoenix. We were so happy to get to
the New Mexico sign as shortly after we were through the storm. This storm made the
List of Derechos on Wikipedia and
has its own
page for the one we drove through.
What was most frightening is that we missed the main part of the storm!
Continue to Mayo Clinic