Prostate Cancer
A Lifetime of Good Health Ends
Mayo Clinic
 It was going to be a very special birthday in March as I turned 65. That meant as of March 1st I could start Medicare. While I was still in
WI by the end of January, I had already set up everything. I signed up for Medicare parts A and B, plus a supplement. So on March 1st I
could now get medical care while we are in Arizona. We had many friends who live with us in Terravita say how great the Mayo Clinic is. It
would be great to get in and see what they had to say about my situation with trying to get this prostate cancer addressed, but we were also told
it's very difficult to get in, and then next to impossible if all you have is Medicare.* But this didn't deter Debbie from trying. We were told
they do like challenging cases and Debbie simply laid out what had happened so far and against the odds I was accepted!
It was going to be a very special birthday in March as I turned 65. That meant as of March 1st I could start Medicare. While I was still in
WI by the end of January, I had already set up everything. I signed up for Medicare parts A and B, plus a supplement. So on March 1st I
could now get medical care while we are in Arizona. We had many friends who live with us in Terravita say how great the Mayo Clinic is. It
would be great to get in and see what they had to say about my situation with trying to get this prostate cancer addressed, but we were also told
it's very difficult to get in, and then next to impossible if all you have is Medicare.* But this didn't deter Debbie from trying. We were told
they do like challenging cases and Debbie simply laid out what had happened so far and against the odds I was accepted!
* I would find out much later that getting into the Mayo Clinic with Medicare was either fairly easy or impossible. They don't have a problem with the coverage I have: Parts A and B and a supplement. What they absolutely refuse is Medicare Advantage plans. I learned why: the insurance companies administering those "advantage" plans will often deny coverage. The Mayo has the luxury of not needing more patients so don't need to go through that hassle.
The Mayo Clinic has two large facilities in Arizona: one in East Scottsdale and the other in North Phoenix. The Scottsdale location is just 35 minutes away and was the original campus when it opened. The North Phoenix campus is just over 20 minutes away and started with a single building that was labeled Mayo Hospital. I remember my mom saying that they built that so they could add 2 additional floors in the future. I was positive she couldn't have that fact correct, but sure enough, 3 years after opening they added those two floors! They would add two more buildings in time. Today it's labeled Mayo Clinic, but that's still the hospital facility.

The North Phoenix Campus of the Mayo Clinic located on Mayo
Boulevard. The hospital building is at the right, the middle is the
Specialty Building, and left one is the Mayo Clinic Building which
contains the cancer center.
So I got an appointment on March 30th with a urologist that turned out to be a surgeon: Dr. Abdul Khan. He was armed with the 90 pages of medical reports from my provider in WI to get their opinion. I was told my original urologist that expect a bias: surgeons will recommend surgery and radiation oncologists will recommend radiation which is what happened in WI. So naturally I expected the same. Dr. Khan was supremely confident in his ability and went through specific detail about the surgery that I didn't get from the doctors in WI. This included a drawing he made of the prostate and how he carefully tries to save the nerves so I have a better chance of keeping sexual function. He was not coming off as arrogant but simply confident. I would be happy for him to be my surgeon and found out later Debbie felt the same. Then I got surprised.
"You have other options"
When it came to my situation, however, he wavered and clearly didn't like the back story of what had happened. He said if I still wanted surgery I'd have to see their cardiologists and their anesthesiologists and even then, he said there was a still a good chance that the anesthesiologist would also shutdown the procedure if they saw the same anomaly in the EKG. And then he said something a little shocking when he added, "I think this is unacceptable when you do have other options." It was confusing that he said options because I thought it was a binary: surgery or radiation. Afterward reading the notes that were made about the visit gave me insight into his thought process. He was under the impression that I wanted to do the surgery when I was genuinely just looking at getting an opinion about retrying the surgery or going down the radiation path. Here's what he wrote:
"This is an extremely pleasant 65-year-old male patient who is known to have intermediate unfavorable risk prostate cancer. He had an attempt prostatectomy at Wisconsin. He reportedly developed ST changes and surgery was aborted. They did not start the actual procedure. They only inserted 3 ports. The postoperative cardiac workup was completely negative. The patient is still interested in surgery. He is here to discuss that."
Out of this meeting I got two appointments for imaging. An MRI of the prostate and a CT scan looking for any other cancer. The CT scan fortunately was negative, but the MRI had one concerning note: "Capsule: Capsular bulge. Curvilinear contact length is 1.8 cm (3/17), There is extension into the retropubic fat anteriorly (7/15) Grade 3." I was worried about this as it seemed to imply the cancer was now getting out of the prostate, but it couldn't because the CT scan was clean.
Over the weekend I thought through my 3 options: Surgery at the Mayo, Radiation at the Mayo, or stay with my surgery date of May 4th in Wisconsin. The last one was a no brainer as there was now no way I'd do the surgery in WI. And though I believed I had a much better surgeon with better support at the Mayo, I decided that the risk was not worth it. That only left radiation as awful as I knew that would be. I messaged Dr. Abdul-Muhsin that I was choosing radiation and in less than an hour I got a call from his assistant that they would put in the referral. There was no, "Are you sure?"
On April 24th, a Tuesday, my MRI appointment was at the Scottsdale Mayo Clinic which is in east Scottsdale, almost to Fountain Hills so a much farther drive, but still only 35 minutes in the morning rush hour traffic. When instructed that portions of the imaging would require that I be especially still, preferably holding my breath and they'd give me the heads up when that was needed. I said it should be no problem because over the only two MRI's, I've had a perfect record of not moving which would require that they'd need to repeat it. I did great as the tech came in the room after it was done he said, "Your perfect record is in tact." The report found the cancer in the prostate, which was hardly a surprise, but there was something new and concerning, a capsular bulge which meant nothing to me. This would be the only appointment at the Scottsdale campus. All the others would be at the Phoenix campus.
 On April 26th, I had a PET CT SKULL TO THIGH PSMA scan. PMSA stands for Prostate Specific Membrane Antigen
and prostate cancer tumors overexpress this protein. To look for this they use the radiotracer
Gallium-68 which has a
half-life of just 68 minutes. Like the
Technetium-99m which was used for the bone scan, it gathers where PSMA
is found so hence finding cancer picked up by the X-ray machine. This is a better technology than the bone scan I received in WI.
The result indicated the cancer had not
metastasized!
On April 26th, I had a PET CT SKULL TO THIGH PSMA scan. PMSA stands for Prostate Specific Membrane Antigen
and prostate cancer tumors overexpress this protein. To look for this they use the radiotracer
Gallium-68 which has a
half-life of just 68 minutes. Like the
Technetium-99m which was used for the bone scan, it gathers where PSMA
is found so hence finding cancer picked up by the X-ray machine. This is a better technology than the bone scan I received in WI.
The result indicated the cancer had not
metastasized!
Radiation Oncologist
I got referred to a radiation oncologist, Dr. Jeffrey Morris, for an appointment on Apr. 27th. He went through the imaging and actually showed some of the MRI images. I couldn't see a thing, even when he pointed to the cancer. And he went over the capsular bulge. It was the bad news I was expecting and the tumor and though it wasn't an absolute certainty, it appears to have breached the capsule of the prostate. He then said there was a good chance that it wouldn't be removed during the surgery. That meant I would need radiation after the surgery. I would have inquired more, but it was irrelevant as I then told him that my mind was already made up that I wasn't going to do surgery. Dr. Morris asked me what I learned about radiation and told him what was laid out in WI. He was dismissive about the procedure laid out by the doctor in WI. "That is rather old and we now have better and faster procedures available. We've learned they can deliver a lot more radiation per treatment." I then learned why the surgeon specifically said options. They have 4 week and 8 week options, 5 times a week, depending on the situation with the cancer in the patient. I also heard something about a 5 treatment plan, but he was offering nothing more specific. Debbie didn't hear this at all! He also mentioned radiation seeds, but did not recommend it for me. Everything would depend on a couple of followup visits, but now a 4 week plan was possible so we would be back in WI a full month earlier.
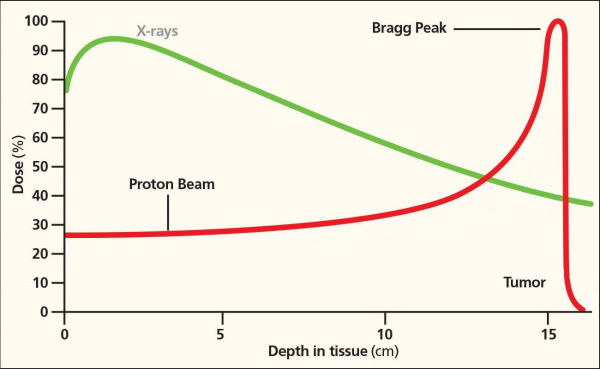 When I was investigating
radiation back in early October, I discovered there was a new technology called
Proton Radiation. Instead of
firing X-rays, protons are used. If you're not familiar, a proton is simply a hydrogen atom with its electron stripped. It's incredibly small.
They are what they
fire in the large particle accelerators where they get them to very close the speed of light and then make them collide with other particles.
But these are not nearly so fast.
The advantage of a proton beam is clearly shown in the diagram at the left. The energy is mostly delivered just before the particle stops and the drop off
is very fast. This is dramatic and especially when compared to the X-ray curve where most of the energy is delivered mostly when it enters body
and doesn't fade much after it goes beyond the tumor. The result of this is that there is a lot less collateral damage. Also, the effective radiation
dose with proton is higher.
When I was investigating
radiation back in early October, I discovered there was a new technology called
Proton Radiation. Instead of
firing X-rays, protons are used. If you're not familiar, a proton is simply a hydrogen atom with its electron stripped. It's incredibly small.
They are what they
fire in the large particle accelerators where they get them to very close the speed of light and then make them collide with other particles.
But these are not nearly so fast.
The advantage of a proton beam is clearly shown in the diagram at the left. The energy is mostly delivered just before the particle stops and the drop off
is very fast. This is dramatic and especially when compared to the X-ray curve where most of the energy is delivered mostly when it enters body
and doesn't fade much after it goes beyond the tumor. The result of this is that there is a lot less collateral damage. Also, the effective radiation
dose with proton is higher.
But you can probably guess the downside. These are very big units which are quite expensive and there are not a lot of these in operation in the United States. Also, studies of the effectiveness of proton vs. X-rays (also referred to as photons) so far do not show any statistical advantage in patient survival. I don't find this surprising because they're both delivering radiation. Your cells normally grow and divide to form new cells, but cancer cells grow and divide faster than most normal cells. Radiation works by making small breaks in the DNA inside cells. These breaks keep cancer cells from growing and dividing and cause them to die. Nearby normal cells can also be affected by radiation, but most recover and go back to working the way they should. However, proton logically will result in fewer side effects. There are a few studies that seem to confirm this, but there are still no longterm controlled studies. All of this was sad to me because it made me wish that had just gotten this prostate cancer later, this would have been my preferred course.
 A week later, however, I would learn from a friend that the Mayo Clinic did in fact have a proton radiation unit because he had received it!
He described it as a 3 story
high structure and they have 4 stations underneath (the picture at the left shows one of them) where they can direct the proton beam.
That way they always have a patient ready when the
proton beam is available. It is in Building 3 of the Mayo complex in North Phoenix. Had I driven by just a few years earlier, I would have
seen it because it was originally called the Proton Building. At the time, however, I thought that I might not qualify for proton because I
only had Medicare, plus the supplement, or it just might not be appropriate for my condition, although I couldn't see why.
A week later, however, I would learn from a friend that the Mayo Clinic did in fact have a proton radiation unit because he had received it!
He described it as a 3 story
high structure and they have 4 stations underneath (the picture at the left shows one of them) where they can direct the proton beam.
That way they always have a patient ready when the
proton beam is available. It is in Building 3 of the Mayo complex in North Phoenix. Had I driven by just a few years earlier, I would have
seen it because it was originally called the Proton Building. At the time, however, I thought that I might not qualify for proton because I
only had Medicare, plus the supplement, or it just might not be appropriate for my condition, although I couldn't see why.
Had I read the notes in MyChart (which Mayo calls "Patient Portal") of Dr. Morris' report, things would be a lot clearer. There was actually quite a bit that he said he went over during the appointment, that he either didn't say or I completely missed. But the big difference in the notes is that a doctor can be very technical which would be difficult in a regular appointment because things would be hard to explain. Here's a passage from that report:
"ASSESSMENT AND PLAN: 65 y.o. with adenocarcinoma of the prostate T3a,N0,M0 GS 7 PSA 9.4"
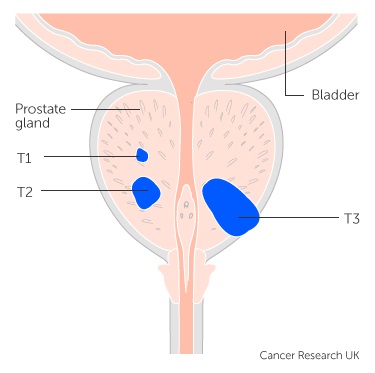 So cancer of the prostate. The other string of gobbledygook I translate from my research:
So cancer of the prostate. The other string of gobbledygook I translate from my research:
- T is Tumor: T3a means the cancer has broken through the capsule (covering) of the prostate gland. Sadly, I had no idea at the time how serious this was, and I swear I never heard the doctor saying anything about it.
- N is Node: N0 means that the nearby lymph nodes don't contain cancer cells.
- M is Metastasis: M0 means the cancer hasn't spread to other parts of your body.
- GS is Gleason Score: 7 which in my case is 4+3 which is unfavorable intermediate risk.
- PSA is straightforward. My most recent measurement of my PSA is 9.4.
Then the next two lines were as follows:
"Discussed options for moving forward which include radiation, surgery, and watchful waiting.
Recommended protons for 5-20 treatments and androgen deprivation for 18 months."
The Paths of Possible Treatments
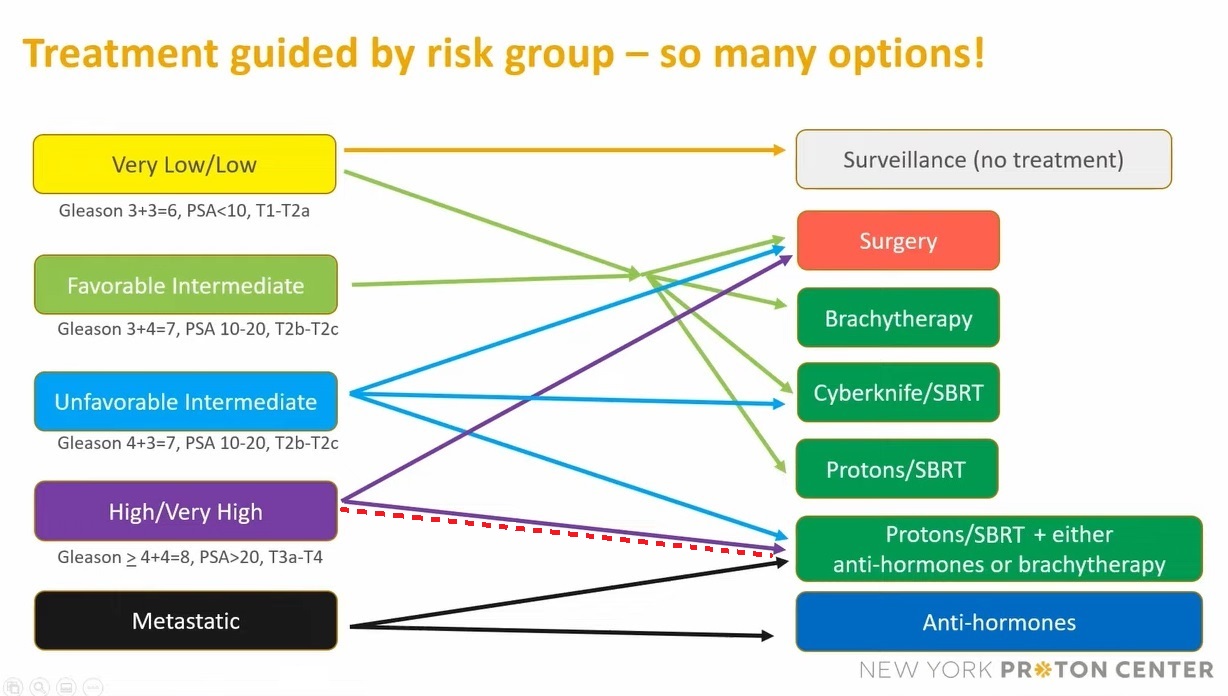
From the chart above based on my Gleason score of 4+3=7 I would be categorized as Unfavorable Intermediate, but my T Staging of T3a puts me into the nasty category of High/Very High. I've highlighted my path from High/Very High with the dashed red line. And as you can see in this category means my radiation needs to be supplemented with Anti-hormones (i.e., ADT, Hormone Therapy).
Preparation For Radiation Treatments
It was some 5 days later when I got a phone call from a nurse that a bunch of appointments had been for Tuesday, May 16th, and Thursday, May 18th, 4 the first day and 5 the second day. All of these were prep for the radiation treatments. The reason for the call was she needed to discuss the what was needed for the appointment on the 16th. I would need to do a Fleet enima 2 hours before and arrive with a full bladder.
May 16 - Appt. 1 The first appointment on Tuesday was the uroflow test with Nurse Kellie Marabella. The instructions were to come to the appointment with a full bladder and I would relieve myself into a collection container so the amount can be measured. They didn't mention if speed was important, but I assumed it was and I really don't know if they did. I wanted to be done quickly, but it was actually too quick. They then do an ultrasound to see how much urine is left in the bladder. I didn't think I did very well so I was disappointed because this could impact the treatment regimen.
May 16 - Appt. 2 This was just a blood Test for PSA. The reading 10.3 which was slightly higher than my previous 9.4. Small fluctuations in the PSA are normal.
May 16 - Appt. 3 A quick visit with Nurse Kellie Marabella where I received a Rocephin [an antibiotic] injection and vitals prior to seed placement appointment that would follow.
May 16 - Appt. 4 This procedure was called "URO Seed placement - prostate - fiducial markers" and was performed by Dr. Gavin Hughes.The procedure was nearly identical to the prostate biopsies (going through the rectum which is why the Fleet enema was required) except there were no audible clicks that you heard when a sample was taken. Instead, Hughes, guided by ultrasound placed 4 metal markers the size of a grain of rice. The procedure was almost entirely painless. The only thing I really felt was the lidocaine injection. Really, ironic that it's for the suppression of pain. He had another doctor with him who I learned is a resident learning the procedure. Only now and then did I hear comments he was giving to the student. When we were done he asked me how I thought it went and I said it was great. I then added that only if he needed to get near the apex would there really be a problem because that is very difficult to reach. He then asked me if I was a medical professional and I answered no, but I have prostate cancer and I've done my own research. I thought of this later and it made me think he didn't check or didn't remember my tumor was at the apex of the prostate. He would then have known I had a biopsy of it so would know that it is difficult to access.
May 16 - Appt. 5 This an unscheduled appointment and was supposed to be a quick meeting about participation in a study. It was never rescheduled because I learned much later it was a study by my radiation oncologist, Dr. Vargus! But looking at the study criteria I wouldn't have qualified as I would have needed to be on a 20 treatment regimen.
May 18 Appointments. As prep for this day I needed to give myself a Fleet enema for the CT Scan.
May 18 - Appt. 1 This appointment was with Nurse Camille. She went through everything and acted like this was just a review. But one of the first things she said was I'd be receiving just 5 treatments of Proton Radiation! Unbelievably great news so the uro flow was not as bad as I thought. I let her know how happy I was to receive that news. She also said I'd be receiving Androgen Deprivation Therapy (ADT) which will reduce my levels of male hormones, called androgens, in my body which will help because they fuel prostate cancer cell growth. The main androgens in the body are testosterone and dihydrotestosterone (DHT). This did not surprise me because it aligned with the research I had done and various guys that I talked to in Terravita that had prostate issues.
May 18 - Appt. 2 The second appointment was the CT Simulation. Immediately I was given a bottle of water that I needed finish as quickly as possible because a fairly full bladder would be needed for the upcoming CT scan in approximately 45 minutes. I needed to get into a gown. Their description of the procedure: "A CT (Computed Tomography) scan imaging technique used to obtain detailed internal images of the body utilizing x-rays." The simulation is they go through the steps for the upcoming real treatments. Here are the steps:
- Immobilizing the body. Here they find a comfortable position that you will be able to keep still for at least 10 minutes. I just needed restraints for my lower legs and I laid directly on my back.
- Imaging. Once I was correctly positioned, the radiation therapy team took CT images of the area of my body to be treated. This helps the radiation oncologist determine the exact areas where treatment will be focused. To help with positioning they had me hold a 6-inch foam ring with both hands. Apparently I did well holding still.
- Marking. To indicate the area where radiation should be aimed, the radiation therapy team used a combination of laser lights and marks on my body. This also ensures that my body is precisely aligned and positioned properly for each treatment session.
-
 Tatoos. Three tiny tattoos, small dots of ink under the skin
are permanent marks that
can't be accidentally rubbed off or washed away, were then placed. This photo shows how small the tattoos are
which is
about the size of a freckle. They were put on very fast and I could
only see where one of them was, and the other two I could only feel
going on. There was really no pain at all. Later, I could only find the
one I saw being placed.
Tatoos. Three tiny tattoos, small dots of ink under the skin
are permanent marks that
can't be accidentally rubbed off or washed away, were then placed. This photo shows how small the tattoos are
which is
about the size of a freckle. They were put on very fast and I could
only see where one of them was, and the other two I could only feel
going on. There was really no pain at all. Later, I could only find the
one I saw being placed.
I was very encouraged coming out of this precedure that the actual treatments would be no problem.
Looking at the notes in MyChart it said that the target was "Prostate + SV" which means the Seminal Vesicles will be irradiated along with the Prostate.
May 18 - Appt. 3 With Nurse Lilyanne Gatterdam. This was short because I would just get a glucagon injection 0.5-1 mg (GlucaGen). Of course I had no idea what that was and why I needed it, but I learned later. Glucagon is a hormone made in the body that increases blood sugar levels. Glucagon was used during an MRI to slow down the motion in the bowels. This enables clearer pictures of the stomach and pelvis areas.
May 18 - Appt. 4 MRI of the prostate. This was another procedure that I needed to be fully hydrated. This would turn out to be the most uncomfortable appointment of any other. I immediately downed a bottle of water in anticipation, but soon learned they expected a small delay. I was in a new waiting room and Debbie was not with me. I didn't think she could come along, but there was no time after the CT scan and then the MRI would be fairly quick. But as time went on ... and on ... and on ... I could have got her even though I was still in the gown, but I kept thinking that any second I'd be called. Eventually I had to go to the bathroom which meant I needed to drink more water. This process repeated itself 4 times! I would eventually find out the delay was because there was a problem with the MRI machine. But finally they had it fixed and I was called and so grateful because I really needed to go to the bathroom. But the prep time was took longer and then when I got up on the table they needed to insert an endorectal coil, a thin wire covered with a latex balloon which is then inflated which also pushes against the bladder. The consequence was the urge to pee got worse! They then were ready to start the imagine, but said it was going to take about 12 minutes. I wasn't sure I could hold on that long, but I'd simply have to. The procedure seemed to never end as going to the bathroom was just about my only thought. I started counting down to help pass the time. 12 minutes is 720 seconds. Some time had passed so I started at 600 seconds. The techs came into the room and I hear, "We're done, " and the mini nightmare was over.
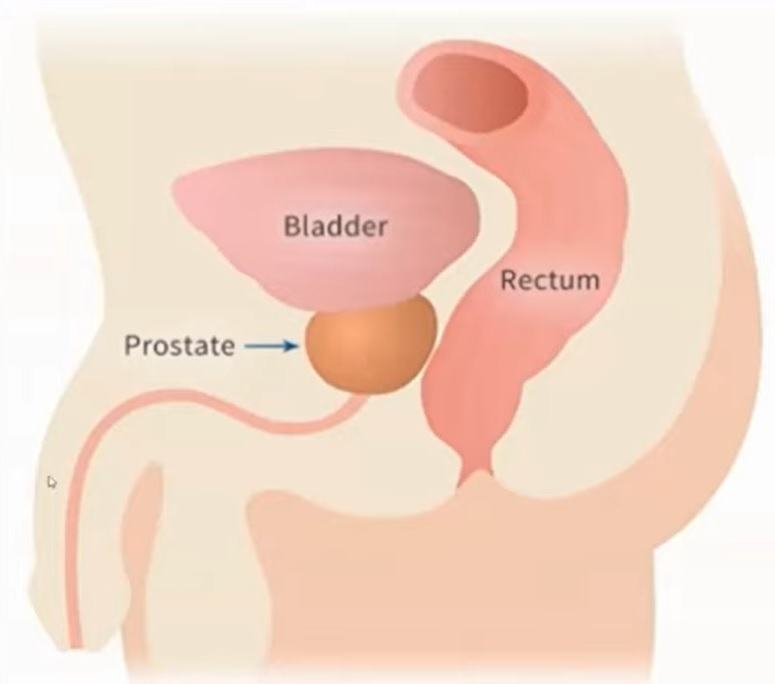 I would not learn until long after the radiation treatments the whole reason why you needed to have a full bladder and then the endorrectal coil (inflated
after insertion). The prostate moves around. Not just between treatments, but even during the treatments! They know the position of the prostate via a
CT which detects the fudical markers. But then the full bladder and rectal balloon press against the prostate to help keep it motionless.
The diagram at the left shows the proximity of the bladder and rectum to the prostate.
I would not learn until long after the radiation treatments the whole reason why you needed to have a full bladder and then the endorrectal coil (inflated
after insertion). The prostate moves around. Not just between treatments, but even during the treatments! They know the position of the prostate via a
CT which detects the fudical markers. But then the full bladder and rectal balloon press against the prostate to help keep it motionless.
The diagram at the left shows the proximity of the bladder and rectum to the prostate.
May 18 - Appt. 5 Visit with Nurse Angie F. I received a 45 mg, 6-month, Leuprolide Acetate injection in the right upper abdomen. This is what they call Androgen Deprivation Therapy (ADT) which lowers testosterone and dihydrotestosterone (DHT). which fuels prostate cancer. In retrospect, I had no idea about the awful side effects.
At the end of the day I received a phone call from Dr. Morris, but missed it because of course my ringer was set to silent. I tried to hear his message but it was inaudible and I couldn't even understand the phone number I was to call. The phone number that was listed was just a general Mayo Clinic number. So I sent him a message through MyChart and the following day he called again. He was concerned that that the uroflow showed a slow peak and some retention. We will start Flomax 0.4 and we will do the 5 treatments. So his call was the need to start a Flomax prescription. Obviously I had dodged a bullet in that I almost didn't qualify for the 5 treatment regimen, but now I was concerned that my urination might be hit hard.
Radiation Treatments
I would only have to wait 4 days to receive the schedule of radiation treatments. The procedure was officially called ProstateSBRT, where SBRT stands for Stereotactic Body Radiation Therapy. I would be receiving just 5 treatments, every other day not including weekends, starting on May 31st. SBRT is a very new but proven technology to position a patient and precisely deliver radiation to a tumor. What was special is that the Mayo Clinic is only the second proton facility that has this technology available.
 May 31st - 1st treatment Wednesday. This will be the most challenging of my 5 visits simply because I hadn't learned how to best handle
coming with a full bladder without it feeling too full. I checked in and soon a tech came to take us back where Debbie was left in the waiting
room while I was taken to the changing area which has at least 16 changing units with a numbered key so your stuff is protected. That area
has its own restroom and its own
door to the waiting room. I could keep my shirt and socks I came with, but underwear, pants, and shoes needed to come off and I got a pair of white pants
for the treatment. I was told that this is how it's going to work for all the treatments and subsequent visits I'd just come and do this myself.
Sounded simple enough. Since I was with Debbie I gave her the key. Otherwise you bring it into the lab.
May 31st - 1st treatment Wednesday. This will be the most challenging of my 5 visits simply because I hadn't learned how to best handle
coming with a full bladder without it feeling too full. I checked in and soon a tech came to take us back where Debbie was left in the waiting
room while I was taken to the changing area which has at least 16 changing units with a numbered key so your stuff is protected. That area
has its own restroom and its own
door to the waiting room. I could keep my shirt and socks I came with, but underwear, pants, and shoes needed to come off and I got a pair of white pants
for the treatment. I was told that this is how it's going to work for all the treatments and subsequent visits I'd just come and do this myself.
Sounded simple enough. Since I was with Debbie I gave her the key. Otherwise you bring it into the lab.
As I entered the waiting room, immediately at the right was a bell that is supposed to be rung at the finish of your treatments. Though seen previously, it didn't mean anything to me. But now I instantly recognized it as a bell from Arcosanti. Me and Debbie visited Arcosanti for the very first time 9 days previous! And we purchased a bell. I knew right then and there I'd be ringing that bell with my last treatment.
 Within 5 minutes my name was called and I was taken by a tech whose name was Colton who escorted to me to Lab #3. I confirmed with him that there
were 4 of them. What was unusual was that there was a long corridor leading from the main hallway to the actual lab. But knowing there were
3 other treatment rooms it made sense. As was the case
with every lab I'd been to over the last 2 years you first walk through a control room that always looks like a scaled down television show
control room, except there were no windows into the treatment room, not surprising given the radiation shielding needed.
The treatment room was a complete surprise as I had nothing pictured in my mind. There were some familiar items, but the most familiar
was the table where I would lie down. The picture at the left shows what it looked like. The big machine at the right was a little confusing
as I thought it was where the radiation would come from, but the position didn't make sense.
Within 5 minutes my name was called and I was taken by a tech whose name was Colton who escorted to me to Lab #3. I confirmed with him that there
were 4 of them. What was unusual was that there was a long corridor leading from the main hallway to the actual lab. But knowing there were
3 other treatment rooms it made sense. As was the case
with every lab I'd been to over the last 2 years you first walk through a control room that always looks like a scaled down television show
control room, except there were no windows into the treatment room, not surprising given the radiation shielding needed.
The treatment room was a complete surprise as I had nothing pictured in my mind. There were some familiar items, but the most familiar
was the table where I would lie down. The picture at the left shows what it looked like. The big machine at the right was a little confusing
as I thought it was where the radiation would come from, but the position didn't make sense.
A tech asked me what music I would like to hear during the procedures. My assumption is they want you to remain calm so hearing something soothing will help. But I couldn't help but be a little sarcastic as I wasn't worried a bit. I told him I'd like the sound of an MRI with the loud thumps because I told him with every MRI I've been I've wanted to fall asleep! Sadly, but predictably, that wasn't on the play list. I don't remember what I actually chose and in the end it didn't matter because you could hardly hear it during the procedure.
Beforehand I had no real expectation about the procedure. I figured I'd just lay there and they zap you with a bunch of radiation. For regular x-ray radiation I would have expected shielding around the target area, but with proton I figured it would not be necessary and I was correct. You walk over to the table and you remove the pants (socks and shirt remain on) and get on the table. I then got an unpleasant surprise as they then needed to insert an endorectal coil, a thin wire covered with a latex balloon which is then inflated which also pushes against the bladder. So since I already felt the need to urinate, this made it worse. It was bad times 5 because I knew that meant it would be done for every treatment. But it's good because 1) it helps protect the rectum from the radiation, and 2) it help keeps the prostate from moving. Once you're into the leg restraints you don't move and to help they give you the 6-inch foam ring I used during the simulation which I held onto with both hands. They then move you into the needed position, and you are instructed not to help. I now really had to urinate and hoped we'd get going immediately. When you're ready the techs vacate the treatment room and over the intercom I get the unwelcome report that I was third in line for the beam. Fortunately it seemed like it was only a few minutes when they said, "We're going to start."
 I was a little bewildered during the actual procedure when I was actually receiving the radiation. The huge machine which was on a
gantry started to move and rotated up into position above me
for maybe 15 seconds and in the middle of that I felt the table shake and 15 seconds later
rotated back out of the way. This is the big structure in the picture at the right. The "garage door"
moves when it moves. Then 3-4 minutes later the table rotated 180 degrees and the big machine rotated again up again for another 30 seconds and, again, in
the middle I felt the table giggle and finally it then backed out of the way. I would find out later by looking it up that the big machine
was simply a standard x-ray imager used to make the final positioning for the actual proton beam. I never felt anything and I couldn't hear anything.
It was as if nothing happened! The techs came into the room and announced that I had done great. I was relieved that the treatment was over so I could
relieve myself.
I was a little bewildered during the actual procedure when I was actually receiving the radiation. The huge machine which was on a
gantry started to move and rotated up into position above me
for maybe 15 seconds and in the middle of that I felt the table shake and 15 seconds later
rotated back out of the way. This is the big structure in the picture at the right. The "garage door"
moves when it moves. Then 3-4 minutes later the table rotated 180 degrees and the big machine rotated again up again for another 30 seconds and, again, in
the middle I felt the table giggle and finally it then backed out of the way. I would find out later by looking it up that the big machine
was simply a standard x-ray imager used to make the final positioning for the actual proton beam. I never felt anything and I couldn't hear anything.
It was as if nothing happened! The techs came into the room and announced that I had done great. I was relieved that the treatment was over so I could
relieve myself.
I then had a very quick visit with Dr. Vargus for the purpose of answering any questions I had. My big question was what would happen after my 5th treatment in terms of follow up. He said he'd see me next November! That meant we could return to WI anytime afterward. The reason is it would take that long before they could get any reliable diagnosis as to the success. At that time they'll get an updated PSA and another 6-month testosterone lowering shot. This would be the longest visit time as the next 4 would take 30 to 40 minutes from the time I arrived until I left the building.
June 2nd - 2nd treatment Friday. I experienced no discernable side effects from my first treatment. I played tennis the day before and that was fine. But this treatment was going to be different because earlier in the morning I drove Debbie to the airport as she was going to Wisconsin to visit family and wouldn't be back until Monday. I had a backup plan of being driven to the appointment had I felt I shouldn't do it alone, but I felt great. Arriving at the desk to check in I was asked, "Do you know where to go?" which took be a little by surprise, but then rememberd the instructions so I said, "Yes," and headed back. You first go to the cabinets that have the pants in sizes ranging from medium to 2XL. You then select one of the changing rooms with numbered keys in the lock. When Debbie was along I'd only keep my shorts and shoes there, but with me alone my wallet and car key were kept there. As you exited you grabbed the key.
This time I managed the full bladder much better as I knew what was going to happen and when. And in the waiting room I got called almost immediately and once again to Lab #3. I mentioned to the tech, whose name I learned was Sheila, that I didn't know when the beam was on as I couldn't hear anything. She pointed at the wall in front of me and slightly to the left where there were two signs: X-Ray and Proton which will be illuminated when on. I was thinking that the big machine that rotated up to be directly on top of me twice during the treatment was probably a standard X-Ray machine for imaging and specifically to get the positions of the seeds so precise targeting could be achieved. It was a little difficult to see so I asked the techs to let me know when the proton beam is on, although they said you could simply turn your head to see. However, I was not keen on doing that because it might result in my lower torso moving which would be bad. And seeing it was almost impossible after the table rotated. But because I now knew what the big machine was a precursor to the proton beam, I could figure when the beam was on. When the treatment was done, Sheila came in and remembered she was supposed to help me when the beam was on and apologized about that.
As it was with the first treatment, I heard nothing and felt nothing. There was no trouble driving myself home and again I experienced no discernable side effects like difficulty urinating and/or fatigue. I played tennis with my usual Saturday group which is always competitive and I did fine.
June 5th - 3rd treatment Monday. Once again I drove myself to the appointment as Debbie would not be returning until that evening. In the waiting room there were was someone there ringing the bell with at least 3 techs and several what looked like visitors. This ringing of the bell looked like it was a big deal and it was a nice thought I'd be doing it in just a week. For this treatment it was a different tech that got me, but we still went again to Lab #3. As I was about to get on the table I joked with the techs, "I haven't felt anything and haven't heard anything. If I didn't know better I'd swear I'm in a prostate cancer research study and I'm in the control group getting the placebo!" Without missing a beat, Sheila, the tech snaps back, "You're not supposed to know that!" From the speed of the response I knew she'd heard this before. But I was so stunned I didn't have the perfect comeback which would have been, "And you are not supposed to know that!" as any reputable study would be done double blind.
I picked up Debbie at the airport, but that evening I struggled a little with the urination. It wasn't awful, but I worried a little that I still had 2 more treatments to go!
June 7th - 4th treatment Wednesday. With Debbie back I still drove but she came along and would be in the waiting room. Once again I was escorted to Lab #3 which prompted a question, "Does a patient always get in the same treatment room?" The tech said that is generally true, but not always and it depends on availability. This time I was able to see out of corner of my eye when the X-Ray light was on and when the proton beam was on. I now had the routine of arriving with a full bladder down to practically a science. I would stop drinking 30 minutes before arriving. Now with the insertion and inflating the balloon, it wasn't too uncomfortable.
That afternoon and into the evening I noticed that my urination seemed to be much improved. I was still having more difficulty than I'd had before, the radiation began, but I was jazzed that I only had one more treatment.
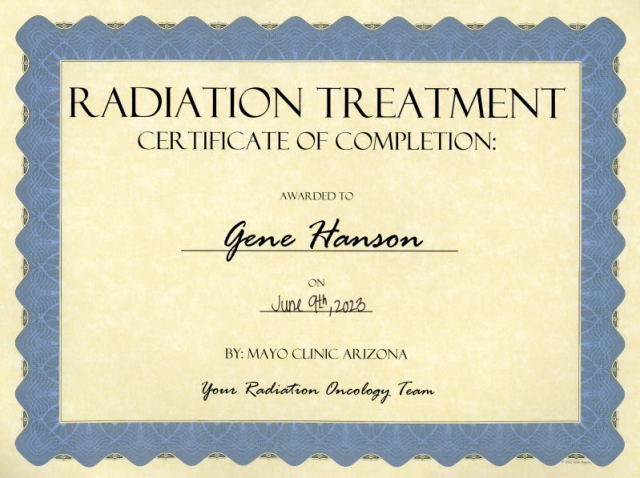
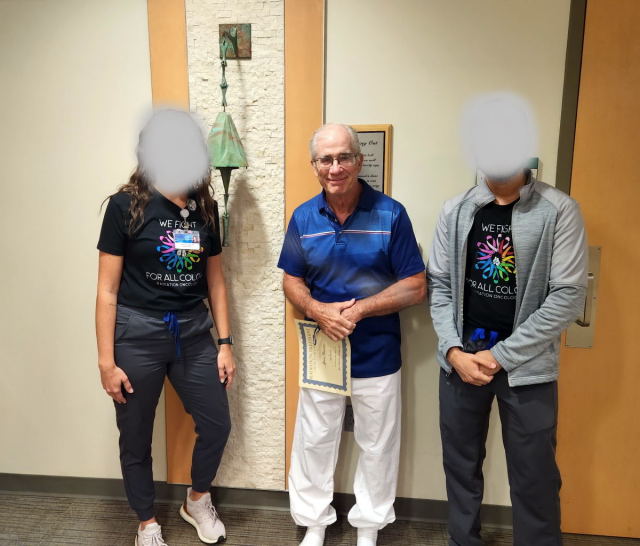
June 9th - 5th treatment The day of the last treatment had arrived. I expected the treatment would be exactly the same as the previous four, but this time I would ring the Arcosanti bell. It was the last time I would intentionally leave the house with a full bladder. It would be the last time I would get a coil with latex shoved up my ... That was reason enough to celebrate. Once again it was Colton that got me and again I would be in Lab #3 and the other tech was Sheila. The treatment of course was exactly the same as the previous four with two exceptions. The first was they immediately acknowledged that this was my last treatment. The second came when the radition was complete. They had a couple of gifts for me: a certificate of completion and a very nice medalion that I immediately thought would be perfect as an ornament on our Christmas tree. Then they said, We'll be in the waiting room in a few minutes for the bell ringing." No questions asked, it was just standard procedure.
I wasn't sure I had enough time to change from my treatment pants, so I waited for the techs to show up.
Aftermath
Since I would not have a follow-up until November, after my last treatment I was ready to go back to Wisconsin for the rest of the summer. But Debbie thought we better wait at least a week to be sure there were no side effects. Frankly, the only thing I worried about was needing to urinate too frequently because you can be trapped in the car for long periods between rest stops. So we waited a week and feeling no side effects (plus urination was actually doing better) we headed out of Arizona on June 19th.
But by the end of June the side effects of the Androgen Deprivation Therapy (ADT) would rear its ugly head. I was still suffering from the inflammation, but things just got worse. I felt fatigued all the time and in particular my legs felt heavy. I was supposed to exercise, but just didn't feel like it. To me it felt like I had aged 10-20 years.
Here is the list of the side effects. A checkmark indicates I have this, a ? means unknown, and nothing afterward means not experiencing.
- Fatigue ✓
- Loss of interest in sex (lowered libido) ✓
- Hot flashes ✓
- Loss of muscle mass and physical strength ✓
- Weight gain ✓
- Changes in blood lipids ✓
- Mood swings ✓
- Impaired memory and attention ✓
- Hair loss✓
- Erectile dysfunction
- Growth of breast tissue
- Anemia
- Loss of bone density ?
- Bone fractures ?
- Insulin resistance ?
- Increased risk of cardiovascular disease ?
I have seen this list in over a dozen forms, but there is one item that I've never found: ADT is a persistent reminder that I'm suffering from prostate cancer. Perhaps it's considered a part of Mood Swings, but more likely it's because it's an amalgamation of many of the other effects. For me it's the absolute worst side effect of prostate cancer.
After our return in early June to Wisconsin, I scheduled an appointment with the cardiologist I was assigned after the surgery, Dr. David Nguyen, and saw him in early July. I was supposed to have the follow-up 2 months after, but I was in AZ and really wasn't all that concerned with my heart given the results of the catheterization. I was anxious to get some follow-up thoughts about the surgery and my subsequent decision to opt for radiation. But I would be bitterly disappointed. When I mentioned my radiation he was visibly confused and I could see he had no idea what I was talking about. It was clear he hadn't checked my chart before the appointment to remind him why I was his patient! He would, however, after the appointment consult his charts and in his report he made it sound like he knew all about the radiation.
Two weeks later I had an appointment with my PCP, Dr. Smith, who got the proton radiation into my charts. I asked him about my mild cardiac disease and if there was really any big concern and he assured me that the level of calcification was completely normal for a 65 year old. He said words to the effect that based on just my heart I'd live well past 90.
Back in AZ I got a message that I should call my radiation oncologist about a follow-up appointment that he wanted 6 months out. I called and the appointment was on November 17th, almost exactly 6 months from the date I received my 6-month injection for ADT. It was actually 3 appointments: (1) A blood test to measure my current PSA, (2) a consultation with Dr. Morris' PA, and (3) another 6-month ADT injection. There was no prep needed. I would just show up. Debbie, of course, came with me and I got the blood test and only a single vile was drawn because only for PSA. The next appointment wasn't until 2 hours later and the reason was obvious: the PSA reading was going to be a big driver of the follow-up appointment so time was built in to assure the reading would be available. So after the test, we went to lunch so we could be back.
While at the restaurant I was expecting a notification of the test result availability, but none came. When we were back at the Mayo Clinic we checked in for the appointment, but still no notification. I decided I would log into the Patient Portal and sure enough, the test result was available. In my mind a couple of scenarios played out. First of all, my last PSA test value was 10.3 at the time the treatments began. That is way too much and the standard range is less than 4.5. But even 4.5 is bad if you've already been diagnosed for prostate cancer. So I was expecting it to be lower than that. Maybe 3? Maybe 2? The reason they wait six months is that it takes time for the value to lower and they really want that value to be less than 1. If it was then it just might need more time for the value to drop.
I "held my breath" as I opened the test to see the result and this is what I saw:
 It was beyond my wildest imagination. The value of <0.10 was essentially zero which meant I was cancer free!
It was beyond my wildest imagination. The value of <0.10 was essentially zero which meant I was cancer free!
But my euphoria was short lived. Note that the value is not shown as zero. It simply means that at the current time it's too low to measure so there still may be some cancer cells remaining. This will lead to the somewhat bad news.
My appointment was with Dr. Morris' PA, Jane Rosenberg and it went as I suspected. She started by asking if I'd seen the test results and I affirmed that I had and I interpreted it correctly: not zero, but simply too low to measure. They thought they knew immediately what my next question would be and, "No, you have to continue the ADT." That was not going to be my question because I already knew the explanation and I knew there was no hope they'd say, "You don't need the ADT anymore!" That would have been wonderful news, but the reason is they don't know there aren't lingering cancer cells remaining and they could grow. The doctor was surprisingly not ready and had no answer to my question, "How low is low? How many cancer cells in a grouping become detectable?" Is it one? Is it 10, 100, 1000, ...? At the end of the appointment I would receive my second 6-month shot of Luprin.
You would think I would not be getting used to the side effects, but my inflammation problem got decidedly worse. I remember at the time of radiation treatments the inflammation had got to the point where it was merely a minor inconvenience. Most of the time I was oblivious to it. But now it was apparent to me most of the time. Putting on sock and shoes were once again problematic and there was always pain doing these simple task. I could play golf, but my swing speed was so much slower which showed by how far a shot would go for any given club. Checking the web I couldn't see any direct connection between the ADT and inflammation, but to me the timing was pretty damning. What I did was now to find out as much as possible about ADT and there were some disconcerting facts. First and foremost being on an 18-month regimen on ADT after surgery or radiation is a long time. More typlically it's 3-6 months. I figured the culprit was my T3a staging meaning the prostate cancer had got out of prostate. Definitely into the seminal vesacles but maybe even beyond that and has metastized.
The other problem with ADT is that if you're on it long enough your prostate cancer cells will become resistant to the low testestore. I learned to fight this you should probably be on intermittent ADT. So you get off of it for a while and then get back on. But this can be driven by your PSA readings. Right now I assumed my PSA was essentially zero so saw no harm getting off of it for a period. I would now have some questions at the next appointment which happened on May 17th. The drill was the same: come in for the PSA test and then 1.5 hours later the appointment with Dr. Rosenberg.
This time I was not surprised that I got another PSA reading of <0.10 so, again, essentially but not necessarily zero. But with that reading I would think I wouldn't need another 6-month shot and should instead start intermittent ADT. But she was holding to her guns about staying on it for the full 18-months, even though he was also saying I might be cured which is their goal. So I then had to ask her point blank: Does this have to do with my T3a staging? She momentarily had the "deer in headlights" look as she wasn't expecting that question. After an awkward pause she finally said, "Yes." So at the end of that appointment I would be getting my third ADT treatment. But there was some good news. She said this was going to be the last shot. What was now going happen is simple monitoring of the PSA at 6-month intervals. If the reading remains essentially zero, life is good and maybe my cancer had been cured. But if the PSA starts to rise (an indication that there are still some cancer cells) they'll let it rise. How long? Until it gets to a level they believe it will show up on a PSMA PET-CT scan. They will then target it with another round of radiation. So in other words a high tech game of Whac-A-Mole.
At this point I don't know the end of the story, but right now it's as good as it gets! But "as good as it gets" is pretty unsatisfying while I endure the ADT. I finally decided I needed to make an appointment with my Rheumatologist while I was back in Wisconsin to see if she had an opinion of what was going on. I would get two new inflammation blood test which showed my levels to be substantically higher than when I saw her two years previous! So the additional pain I was feeling was not my imagination. But when I told her I had prostate cancer was was on ADT she said that would definitely exasperate any inflammation problem! That was good news as it indicated when I would finally be off the ADT my inflammation problem would subside.
| Blood Test | 05/2022 | 08/2022 | 06/2024 |
| CRP | 10.9 | 3.7 | 5.3 |
| ESR | 26 | 6 | 18 |
Stayed tuned. My next appointment is on December 2nd. I don't think anything is going to be different in terms of PSA, but hopefully I will be regaining my testosterone!